Introduction
Chronic kidney disease (CKD) represents a global health challenge, with an increasing incidence of renal failure observed in both developed and developing nations. This condition is associated with significant morbidity and mortality, leading to a marked reduction in patients' quality of life. 1
The eyes often reflect various systemic conditions within the body. With the rising prevalence of diabetes and hypertension in India, paralleling trends in the Western world, the incidence of CKD is expected to increase over time. 2
CKD encompasses a range of pathophysiological processes characterized by abnormal kidney function and a progressive decline in glomerular filtration rate (GFR). This gradual loss of renal function unfolds over several years, often silently. 3
The kidneys' normal functions can be disrupted by various diseases and medical conditions, particularly diabetes mellitus, which is known to cause microvascular complications like diabetic retinopathy (DR) and nephropathy. 4, 5
Chronic kidney disease exerts widespread systemic effects, impacting multiple organ systems, including the eyes. Long-standing CKD can lead to ocular changes, and certain systemic diseases, such as diabetes, hypertension, and autoimmune disorders, can concurrently affect both the kidneys and the eyes.6
Ocular manifestations may arise either as a direct consequence of the primary diseases leading to renal failure or as secondary effects of CKD itself. The connection between renal disease and visual impairment was first reported by Richard Bright in 1836.7 The disturbances in fluid and electrolyte balance, coupled with the underlying comorbidities frequently observed in CKD patients, elevate the risk of various ocular abnormalities that can significantly impair vision.
Material and Methods
This study is a cross-sectional, descriptive, non-interventional, hospital-based study, conducted over a four-month period from May 2024 to August 2024.
The study included patients admitted to the Department of Nephrology who had been diagnosed with chronic kidney disease (CKD) and for whom bedside ophthalmology consultations were requested. A total of 70 patients were enrolled.
The inclusion criteria encompassed patients aged 18 years and older diagnosed with CKD. Exclusion criteria included patients who declined to provide consent, those with reversible causes of renal failure, and individuals who had undergone renal transplantation.
The significance of ocular evaluation in CKD was thoroughly explained to each patient. The examination procedures were detailed, and informed consent was obtained from all participants. Following consent, a comprehensive ocular examination was performed on 140 eyes from the enrolled patients.
Results
In this study, we evaluated a cohort of 70 patients diagnosed with chronic kidney disease (CKD), consisting of 38 males (54.3%) and 32 females (45.7%).(Table 1)
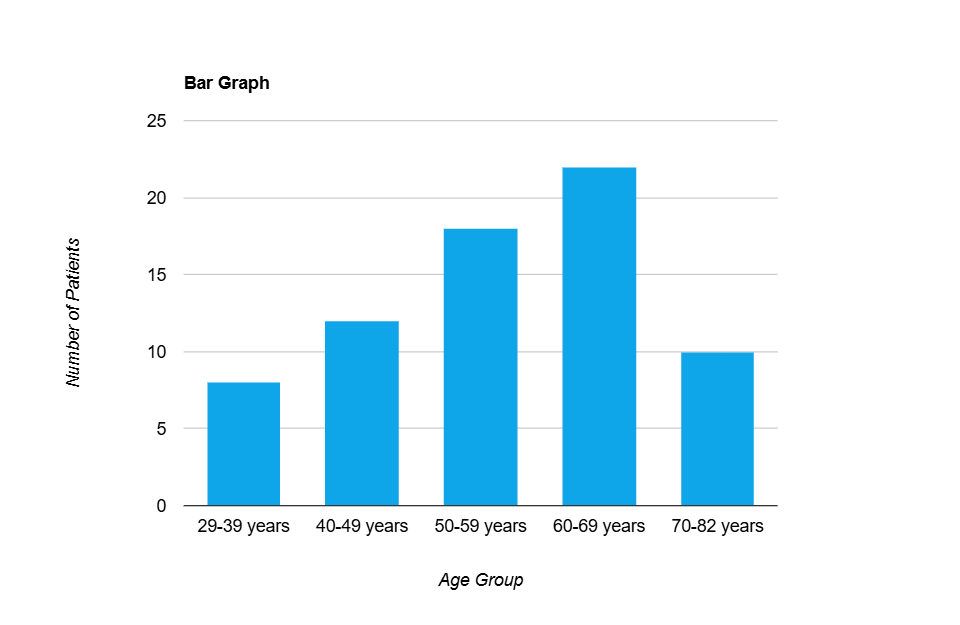
The age distribution ranged from 29 to 82 years, with the majority of patients (31.4%) falling within the 60-69 age bracket.(Figure 1)
Specifically, 22 patients (31.4%) were between 60-69 years, 18 patients (25.7%) were aged 50-59 years, 12 patients (17.1%) were in the 40-49 age range, and 10 patients (14.3%) were between 70-82 years. The smallest group consisted of 8 patients (11.4%) aged 29-39 years.
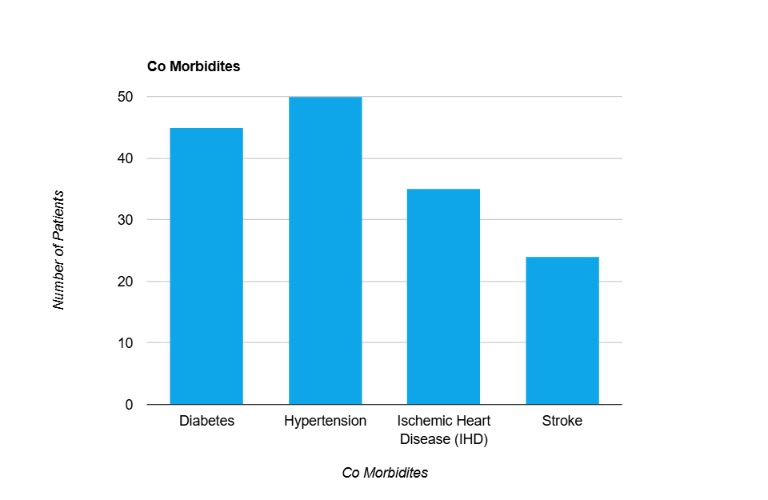
A substantial proportion of patients presented with significant comorbidities. Hypertension was the most common, identified in 50 patients (71.4%), underscoring its role as a major contributor to CKD progression.
Diabetes mellitus was present in 45 patients (64.3%), reflecting its strong association with both nephropathy and retinopathy.
History of stroke was noted in 24 patients (34.3%) Ischemic heart disease was documented in 35 patients (50.0%), highlighting the interconnected nature of CKD with cardiovascular pathology.(Figure 2)
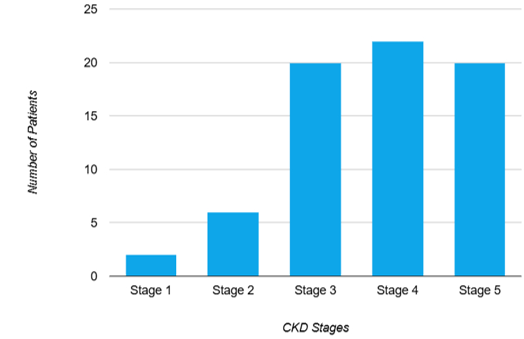
The distribution of CKD stages revealed that the majority of patients were in advanced stages of the disease.
Stage 4 CKD was most prevalent, affecting 22 patients (31.4%), followed by Stage 5, which was present in 20 patients (28.6%).
Stage 3 CKD was observed in 20 patients (28.6%).
While early-stage disease was less common, with Stage 2 found in 6 patients (8.6%) and Stage 1 in just 2 patients (2.9%).(Figure 2)
Lifestyle factors known to exacerbate CKD progression were also documented. Notably, smoking was prevalent among 32 patients (45.7%), while 19 patients (27.1%) reported alcohol consumption, and 27 patients (38.6%) engaged in tobacco chewing.
These habits are known risk factors for both cardiovascular and renal disease, further complicating the clinical picture in this population.(Table 2)
Table 2
Habits
|
Smoking history |
Frequency |
Percentage |
|
Yes |
32 |
45.7% |
|
No |
38 |
54.3% |
|
Alcohol consumption history |
||
|
Yes |
19 |
27.1% |
|
No |
51 |
72.9% |
|
Tobacco chewing history |
||
|
Yes |
27 |
38.6% |
|
No |
43 |
61.4% |
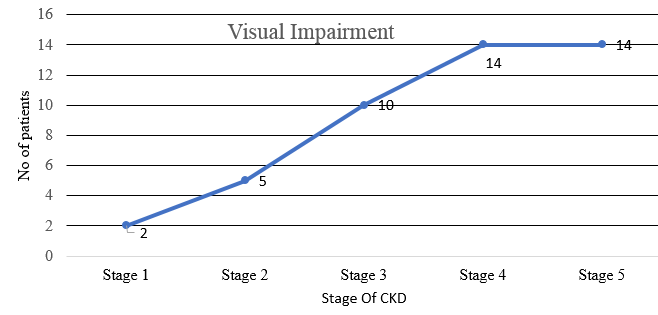
The distribution of visual acuity across the different stages of chronic kidney disease (CKD) reveals a progressive decline in visual function with advancing stages of renal impairment. In CKD Stage 1, the majority of patients (10 out of 12) maintained good vision, reflecting minimal ocular involvement in the early stage of kidney disease. Only 2 patients experienced visual impairment, and no cases of blindness were observed.
In CKD Stage 2, a similar trend was noted, with 8 out of 13 patients retaining good vision. However, there was a slight increase in visual impairment, affecting 4 patients, and a single case of blindness, suggesting the beginning of retinal and other ocular changes associated with mild to moderate renal dysfunction.
As the disease progressed to CKD Stage 3, a noticeable shift was observed. The proportion of patients with good vision decreased to 5 out of 15, while visual impairment rose to 7 patients. Moreover, 3 patients were classified as blind, reflecting the increasing impact of moderate CKD on ocular health, potentially due to associated systemic vascular changes and ocular co-morbidities.
In CKD Stage 4, the data showed a marked reduction in patients with good vision, with only 2 out of 16 maintaining visual acuity in this category. The majority, 9 patients, were found to have visual impairment, and 5 patients were recorded as blind. This stage exhibited a significant increase in severe visual outcomes, correlating with advanced renal dysfunction.(Table 3)
Table 3
Progression of visual impairment with stage of CKD.
|
CKD Stage |
Good Vision ≥6/18 |
Visual Impairment 6/18-6/60 |
Blindness <6/60 |
Total Patients |
|
Stage 1 |
10 |
2 |
0 |
12 |
|
Stage 2 |
8 |
4 |
1 |
13 |
|
Stage 3 |
5 |
7 |
3 |
15 |
|
Stage 4 |
2 |
9 |
5 |
16 |
|
Stage 5 |
0 |
6 |
8 |
14 |
|
Total |
25 |
28 |
17 |
70 |
On examination of the anterior segment using torch light, it was noted that out of the total 140 eyes, 31 eyes exhibited various findings.
Examination of eyelid conditions revealed that a predominant 90% of eyes (126 out of 140) presented with normal eyelid morphology. In contrast, 10% of the eyes (14) displayed various pathological features. Among these, xanthelasma was observed in 4 eyes, accounting for approximately 2.9% of the sample. Sebaceous cysts were noted in 5 eyes, representing about 3.6%, while papillomas were identified in 3 eyes, constituting roughly 2.1%. Nevi were found in 2 eyes, or about 1.4% of the examined population.(Table 4)
Table 4
Eyelid Manifestations
|
Eyelid Manifestations |
Frequency |
Percentage |
|
Normal |
126 |
90% |
|
Sebaceous Cysts |
5 |
3.6% |
|
Xanthelasma |
4 |
2.9% |
|
Papillomas |
3 |
2.1% |
|
Nevi |
2 |
1.4% |
In the conjunctival assessment, 88% of eyes (123 out of 140) exhibited normal findings. The remaining 12% (17 eyes) demonstrated several abnormal conditions. Nasal pterygium was identified in 7 eyes, making up approximately 5% of the total, while biheaded pterygium and pinguecula were each observed in 5 eyes, corresponding to about 3.6% for each condition.(Table 5)
Table 5
Conjunctival Lesions
|
Conjunctival Manifestations |
Frequency |
Percentage |
|
Normal |
123 |
88% |
|
Nasal Pterygium |
7 |
5% |
|
Biheaded Pterygium |
5 |
3.6% |
|
Pinguecula |
5 |
3.6% |
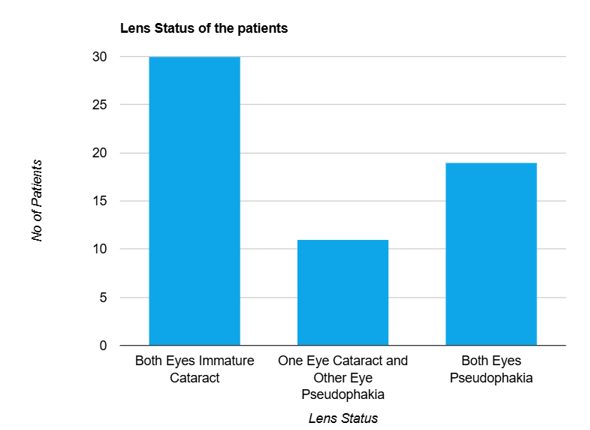
Lens evaluations revealed that 62% of the eyes (87) presented with immature cataract. In comparison, 38% of the eyes (53) were pseudophakic. When further dissecting these findings, it was noted that 30 patients (60 eyes) had immature cataract in both eyes. In a different subset, 19 patients (38 eyes) had pseudophakia in both eyes. Additionally, 11 patients (22 eyes) exhibited a combination of one eye with immature cataract and the contralateral eye with pseudophakia.(Table 6)
Table 6
Lens evaluations
|
Lens Status |
Frequency |
Percentage |
|
Pseudophakia |
53 |
37.9% |
|
Immature Cataract |
87 |
62.1% |
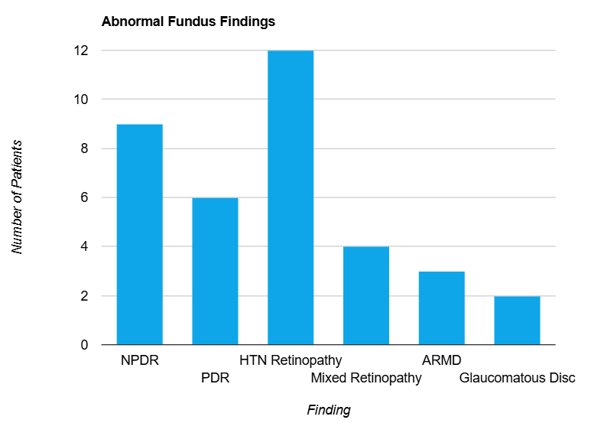
Fundoscopy was performed on all patients to assess posterior segment, revealing that 34 patients (48.6%) had a normal fundus, while 36 patients (51.4%) exhibited abnormal findings. (Table 7)
Table 7
Fundoscopic findings
|
Fundoscopic findings |
Frequency |
Percentage |
|
Normal |
34 |
48.6% |
|
Abnormal |
36 |
51.4% |
The abnormal fundoscopy results were categorized as follows: non-proliferative diabetic retinopathy was detected in 9 patients (12.9%), proliferative diabetic retinopathy in 6 patients (8.6%), hypertensive retinopathy in 12 patients (17.1%), mixed retinopathy in 4 patients (5.7%), age-related macular degeneration (ARMD) in 3 patients (4.3%), and glaucomatous disc changes in 2 patients (2.9%).(Figure 6, Figure 7, Figure 8)
Table 8
Fundus findings in various stages of CKD
The distribution of fundus findings across the different stages of chronic kidney disease (CKD) reveals a progressive increase in the prevalence and severity of retinal abnormalities as the disease advances. Among the 70 patients studied, 34 patients (48.6%) exhibited a normal fundus, while 36 patients (51.4%) had varying degrees of abnormal findings.(Table 8)
In CKD Stage 1, 10 out of 12 patients (83.3%) maintained a normal fundus, indicating minimal retinal involvement at this early stage of kidney disease. Only 2 patients (16.7%) presented with fundus abnormalities, with one case each of non-proliferative diabetic retinopathy and hypertensive retinopathy. These findings suggest that in the initial stages of CKD, retinal changes are relatively uncommon and predominantly mild.
CKD Stage 2 showed a slight increase in the number of abnormal fundus findings. Although 8 out of 13 patients (61.5%) still had a normal fundus, 5 patients (38.5%) exhibited abnormalities. The abnormalities included 2 cases of non-proliferative diabetic retinopathy, 1 case of proliferative diabetic retinopathy, and 2 cases of hypertensive retinopathy. This stage suggests a mild increase in retinal involvement, likely related to the progression of systemic factors such as hypertension and diabetes.
As the disease progressed to CKD Stage 3, there was a more marked decline in the number of patients with a normal fundus, with only 7 out of 15 (46.7%) retaining normal findings. The remaining 8 patients (53.3%) displayed a range of abnormalities: 3 with non-proliferative diabetic retinopathy, 1 with proliferative diabetic retinopathy, 4 with hypertensive retinopathy, 1 with mixed retinopathy, and 1 with age-related macular degeneration (ARMD). This stage reflects the growing impact of moderate renal impairment on retinal health, with a broader spectrum of retinal pathologies becoming evident.
In CKD Stage 4, the number of patients with a normal fundus decreased further to 5 out of 16 (31.3%), while 11 patients (68.7%) exhibited abnormal findings. These included 2 cases each of non-proliferative and proliferative diabetic retinopathy, 3 cases of hypertensive retinopathy, 2 cases of mixed retinopathy, 1 case of ARMD, and 1 case of glaucomatous disc changes. The findings in Stage 4 illustrate a significant increase in both the frequency and complexity of retinal abnormalities, likely driven by worsening systemic vascular damage and metabolic disturbances associated with advanced kidney disease.
By CKD Stage 5, fundus abnormalities became even more prevalent, with only 4 out of 14 patients (28.6%) retaining a normal fundus. The majority (10 patients or 71.4%) exhibited significant retinal pathologies, including 1 case of non-proliferative diabetic retinopathy, 2 cases of proliferative diabetic retinopathy, 2 cases of hypertensive retinopathy, 1 case of mixed retinopathy, 1 case of ARMD, and 1 case of glaucomatous disc changes. This stage, representing end-stage renal disease, demonstrates the highest burden of retinal abnormalities, reflecting the severe systemic impact of CKD on ocular health, including advanced retinopathy and optic nerve changes.
Discussion
The current study highlights a significant correlation between the severity of chronic kidney disease (CKD) and the prevalence and complexity of fundus abnormalities. As CKD progresses, there is a clear trend toward an increasing burden of retinal pathologies, underscoring the close relationship between renal impairment and ocular health. Among the 70 patients examined, fundus findings showed a marked progression from minimal involvement in the early stages of CKD to more severe and varied abnormalities in the later stages.
1. The 2012 kidney disease: Improving Global Outcomes (KDIGO) guidelines categorize chronic kidney disease (CKD) stages according to the estimated GFR (eGFR) calculated from serum creatinine, adjusted for body surface area (ml/min/1.73 m²):
G1: Normal or high function (eGFR ≥ 90)
G2: Mild decrease in kidney function (eGFR 60–89)
G3a: Mild to moderate decrease in kidney function (eGFR 45–59)
G3b: Moderate to severe decrease in kidney function (eGFR 30–44)
G4: Severe reduction in kidney function (eGFR 15–29)
G5: Kidney failure or end-stage renal disease (ESRD) (eGFR < 15)
This classification system is critical for assessing the progression of CKD and guiding appropriate clinical management.
In the recent Screening and Early Evaluation of Kidney Disease (SEEK) 8 cohort study, the overall prevalence of chronic kidney disease (CKD) was reported to be 17.2%. The distribution of CKD across different stages was as follows: stage 1 at 7%, stage 2 at 4.3%, stage 3 at 4.3%, stage 4 at 0.8%, and stage 5 at 0.8%.
Upon comparing the findings of the SEEK cohort study with those of our study, it is evident that both studies provide valuable insights into the distribution of CKD stages in different populations. The SEEK study primarily highlights the prevalence of CKD across various stages in a broad population-based cohort, offering a comprehensive overview of both early and advanced stages. Our study, on the other hand, focuses on a more targeted patient group, providing detailed information on the distribution of CKD stages in a clinical setting.
While the SEEK study outlines a significant proportion of patients in the early stages of CKD, our findings reveal a substantial presence of patients in advanced stages, underscoring the importance of timely detection and intervention.
In CKD Stage 1, the majority of patients (83.3%) maintained a normal fundus, with only a small proportion exhibiting mild retinal changes such as non-proliferative diabetic retinopathy and hypertensive retinopathy. This minimal retinal involvement in the early stage of CKD suggests that, at this point, systemic vascular damage is limited, and any retinal findings are likely mild and confined to patients with underlying systemic conditions like diabetes or hypertension.
As the disease advances to CKD Stage 2, the proportion of patients with abnormal fundus findings increased to 38.5%. At this stage, there is a notable rise in the incidence of both non-proliferative and proliferative diabetic retinopathy, as well as hypertensive retinopathy. These findings may reflect the accumulating impact of systemic conditions such as hypertension and diabetes, which are known to exacerbate retinal changes due to chronic microvascular damage. The moderate renal impairment seen in Stage 2 appears to begin influencing retinal health more substantially, likely due to a combination of increased vascular permeability, endothelial dysfunction, and systemic inflammation.
By CKD Stage 3, over half of the patients (53.3%) displayed abnormal fundus findings, with a broader spectrum of retinal pathologies, including age-related macular degeneration (ARMD) and mixed retinopathy, becoming evident. This stage reflects a critical transition in the disease, where moderate renal impairment increasingly affects retinal health, driven by both the direct impact of renal dysfunction and the compounded effects of co-existing systemic conditions. The growing prevalence of ARMD at this stage further suggests that chronic systemic inflammation and oxidative stress, both hallmarks of CKD, may contribute to degenerative retinal changes.
CKD Stage 4 shows a substantial increase in both the frequency and severity of retinal abnormalities, with 68.7% of patients presenting with various pathologies. Notably, this stage is characterized by a significant rise in more severe forms of diabetic and hypertensive retinopathy, mixed retinopathy, ARMD, and glaucomatous disc changes. The complexity and diversity of retinal findings in Stage 4 may be attributed to the profound systemic vascular changes that accompany advanced renal impairment, such as accelerated atherosclerosis, microangiopathy, and metabolic disturbances. These factors, combined with prolonged exposure to risk factors like hypertension and diabetes, likely drive the increased incidence of vision-threatening retinal pathologies observed at this stage.
By CKD Stage 5, the prevalence of fundus abnormalities reaches its peak, with 71.4% of patients exhibiting significant retinal pathologies. This stage, representing end-stage renal disease, is characterized by the highest burden of ocular complications, including advanced retinopathy and optic nerve changes. The high prevalence of both proliferative diabetic retinopathy and glaucomatous disc changes in this cohort reflects the severe systemic impact of CKD on ocular health, likely mediated through mechanisms such as chronic hyperglycaemia, hypertension, uraemia, and other metabolic derangements. Additionally, the findings of ARMD and mixed retinopathy at this stage underscore the multifactorial nature of retinal pathology in advanced CKD, involving not only vascular and metabolic components but also degenerative processes.
Diabetes is the single most common cause of CKD worldwide, and many patients with diabetes-associated renal failure also have retinopathy. In addition, recent population-based studies suggest that macular degeneration is increased in renal impairment. 9
Risk factors common to renal failure and macular degeneration include increasing age, smoking, and possibly hypertension. 10, 11
The findings of the Atherosclerosis Risk in Communities (ARIC) study, 12 which highlighted a significant association between retinopathy and renal dysfunction independent of traditional risk factors, are mirrored in our study. A parallel trend is observed, with retinal abnormalities becoming increasingly prevalent and severe as the stage of chronic kidney disease (CKD) advances. As renal function deteriorates from early to more advanced stages of CKD, the frequency and severity of retinal findings, such as hypertensive retinopathy, diabetic retinopathy, markedly increase. This progression suggests that worsening renal impairment contributes to the aggravation of microvascular complications in the retina, reinforcing the need for vigilant ophthalmologic monitoring in patients with CKD, especially as they approach the later stages of the disease.
The presence of a diabetic retinopathy is also a marker of increased risk of cardiac disease and death. 13
The analysis of anterior segment findings, such as immature cataracts and pseudophakia, further corroborates the systemic impact of CKD on ocular health. The high prevalence of cataracts among this population is consistent with the known association between renal impairment and increased oxidative stress, which accelerates lens opacification. 14, 15, 16 The presence of pseudophakia in a significant portion of the study population also suggests that many patients had already undergone cataract surgery, reflecting a high burden of vision-impairing lens changes in CKD.
Conclusion
The study highlights the substantial prevalence of ocular manifestations in patients with chronic kidney disease (CKD) and their strong correlation with advancing stages of renal dysfunction. As CKD progresses, both anterior and posterior segment abnormalities become increasingly common and severe, indicating the systemic impact of kidney disease on ocular health. Visual impairment, particularly due to cataracts and retinopathy, is a significant concern in CKD patients, with advanced stages showing a marked increase in blindness and complex retinal pathologies. This study underscores the importance of regular ophthalmic evaluations to detect and manage these ocular complications early, thereby preventing vision loss and improving the quality of life for CKD patients. By demonstrating a clear progression of ocular findings with worsening renal function, this study reinforces the need for integrated care approaches that address both renal and ocular health in managing CKD. The findings suggest that comprehensive ocular assessments should be a routine part of CKD management, particularly in patients with coexisting diabetes and hypertension, to mitigate the compounded risks of microvascular damage and visual deterioration.