- Visibility 124 Views
- Downloads 36 Downloads
- DOI 10.18231/j.ijooo.2024.023
-
CrossMark
- Citation
Recent advances in the management of uveal melanoma
Uveal melanoma is the most common intraocular malignancy in adults, despite it’s low incidence. It gets originated from ocular melanocytes of the choroid (85%), cilliary body (5-8%) and iris (3-5%). It occurs mainly unilaterally in the posterior pole. Uveal melanoma generally have GNAQ or GNA11 mutations and has no environmental risk factors.[1], [2] The median age of presentation is 62 years.[3] The 5 year and 15 year disease related mortalities are 30%and 45% respectively.[4] Irrespective of the treatment of primary tumours approximately half of the patients suffer from metastasis. Metastatic uveal melanoma has poor prognosis, usually fatal after half year of diagnosis. The liver is the most common site of metastasis. The main route of spread is hematological. The main purpose of treating the primary melanoma is to prevent distant metastasis and salvage vision, globe and life of the patients. It can be treated by using radiation therapy, laser therapy, local resection, enucleation and combined procedures. Current preferred mode of treatment is combination of photo therapy, radiotherapy and local tumour resection, depending on the tumour diameter, location and other features such as vitreous haemorrhage, retinal detachment or retinal involvement. [5], [6], [7] Other factors which influences is patient’s age, physical condition, economic conditions and personal preference.
Unfortunately, there is no definitive therapeutic strategies for uveal melanoma with metastasis. Several studies have been conducted which is devoted to target therapy, immune therapy and other newer therapeutic perspectives. Uveal melanoma suppresses both innate and adaptive immunity. In this disease HLA-E which combines with the inhibitory receptor of Natural killer cells is over expressed which leads to the inhibition of the cytolysis procedure mediated by Natural killer cells. Secretion of tumour growth factors at the local site also contribute in inhibition of Natural killer cells and alters it’s susceptibility to uveal melanoma cells. [8], [9], [10]
The recent advances in the understanding of the biology, immunology and micro environment of uveal melanoma have improved prognostication and therapeutic strategies of this deadly disease. Stratification of patients plays crucial role in the development of individualised treatment plans and radiographic surveillance strategies which is done by assessing the risk of metastatic disease following treatment of primary disease using anatomical, clinical and molecular features. Treatment of uveal melanoma is broadly categorised into local and systemic treatment:
There are several recent advances in systemic therapy that acts at molecular level which has very high specificity as it can block the signal transduction pathways and affect the biological behaviour of tumour or stromal cells by acting on specific tumour proliferation related molecules Uveal melanoma with metastasis responds poorly to conventional chemotherapy; targeted therapy can play a role for prospective treatment.
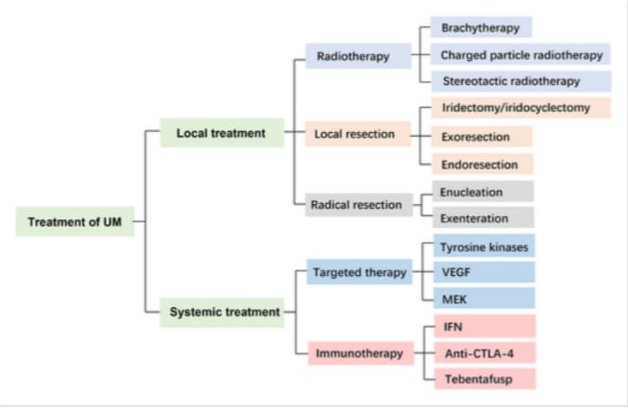
In uveal melanoma T lymphocyte mediated cellular immunity mainly plays a role. Cytotoxic T cells and helper T cells are inhibited by uveal melanoma cells.[11], [12] The upregulation of programmed death ligands (PDL-1) induced by interferon gamma can inhibit T cell activation. So immunotherapy in uveal melanoma should target immune characteristics which includes immune checkpoints inhibitors, cancer vaccines, cell therapy, oncolytic viruses, histone deacetylase inhibitors and their combined treatments. [13], [14]
Immune check inhibitors include drugs like IPILIMUMAB and TREMELIMUMAB. Ipilimumab being the first drug approved for metastatic melanoma therapy by food and drug administration. TREMELIMUMAB is a human monoclonal antibody that targets CTLA-4. This group also includes drugs like Pembrolizumab, Nivolumab and Atezolizumab. [15], [16], [17]
Cancer vaccines includes whole cell based vaccines which activates helper T cells and cytotoxic cells against primary and metastatic Uveal melanoma cells, it also constitutes dendritic cell vaccines which has the most powerful antigen presenting function, so used for stage-4 melanoma. [18], [19]
Immune mobilising monoclonal T-cell receptors against cancer has one drug called TEBENTAFUSP which is the first therapy demonstrated to improve overall survival in patients with advanced stage uveal melanoma. The successful development of this drug highlights the clinical efficacy that can be achieved with appropriate modulation of the antitumor response in this disease. [20]
Some new therapeutic perspectives such as high intensity focussed ultrasound which treats solid tumors in the deep subcutaneous layer via thermal destruction, and aerodynamic therapy which could induce reactive oxygen species were reported to show advantages in treating primary uveal melanoma.
Transcorneal iontophoresis and electrically enhanced chemotherapy increases penetration of anticancer agents are some other novel mechanisms. For small choroidal melanomas drug AU-011 can be used which is light activated molecule and gets activated by diode laser to destroy target cells. [21], [22]
Novel regional therapeutic strategies focussed on uveal melanoma, liver metastasis, systemic targets, epigenetic and immunological treatment and combinatorial approaches are being studied, providing hope for continued progress. Further investigations of the micro environment of UM, clarity of it’s relevant immunological escape mechanisms and determination of effective therapeutic strategy. Advances in the metastatic setting are driving the development of novel adjuvant therapies that might reduce the risk of metastatic spread and increase cure rates for patients with uveal melanoma.
Conflict of Interest
None.
References
- BA Krantz, N Dave, KM Komatsubara, BP Marr, RD Carvajal. Uveal melanoma: epidemiology, aetiology, and treatment of primary disease. Clin Ophthalmol 2017. [Google Scholar] [Crossref]
- C Chattopadhyay, DW Kim, DS Gombos, J Oba, Y Qin, MD Williams. Uveal melanoma: From diagnosis to treatment and the science in between. Cancer 2016. [Google Scholar]
- RT Al-Jamal, N Cassoux, L Desjardins, B Damato, L Konstantinidis, SE Coupland. The Pediatric Choroidal and Ciliary Body Melanoma Study: A Survey by the European Ophthalmic Oncology Group. Ophthalmology 2016. [Google Scholar]
- E Kujala, T Mäkitie, T Kivelä. Very Long-Term Prognosis of Patients with Malignant Uveal Melanoma. Invest Ophthalmol Vis Sci 2003. [Google Scholar]
- F Spagnolo, G Caltabiano, P Queirolo. Uveal melanoma. Cancer Treat Rev 2012. [Google Scholar]
- BA Krantz, N Dave, KM Komatsubara, BP Marr, RD Carvajal. Uveal melanoma: Epidemiology, etiology, and treatment of primary disease. Clin. Ophthalmol 2017. [Google Scholar] [Crossref]
- L Khoja, EG Atenafu, S Suciu, S Leyvraz, T Sato, E Marshall. Meta-analysis in metastatic uveal melanoma to determine progression free and overall survival benchmarks: An international rare cancers initiative (IRCI) ocular melanoma study. Ann Oncol 2019. [Google Scholar]
- X Peng, L Chen, Y Jiao, Y Wang, Z Hao, X Zhan. Application of natural killer cells in pancreatic cancer. Oncol Lett 2021. [Google Scholar] [Crossref]
- M Campoli, S Ferrone. HLA antigen changes in malignant cells: epigenetic mechanisms and biologic significance. Oncogene 2008. [Google Scholar]
- RS Apte, JY Niederkorn. Isolation and characterization of a unique natural killer cell inhibitory factor present in the anterior chamber of the eye. J Immunol 1996. [Google Scholar]
- M Oliva, AJ Rullan, J Piulats. Uveal melanoma as a target for immune-therapy. Ann Transl Med 2016. [Google Scholar] [Crossref]
- FH Durie, AM Campbell, WR Lee, BE Damato. Analysis of lymphocytic infiltration in uveal melanoma. Invest Ophthalmol Vis Sci 1990. [Google Scholar]
- M Radosevich, M Jager, SJ Ono. Inhibition of MHC class II gene expression in uveal melanoma cells is due to methylation of the CIITA gene or an upstream activator. Exp Mol Pathol 2007. [Google Scholar]
- M Radosevich, Z Song, JC Gorga, B Ksander, SJ Ono. Epigenetic silencing of the CIITA gene and posttranscriptional regulation of class II MHC genes in ocular melanoma cells. Invest Ophthalmol Vis Sci 2004. [Google Scholar]
- L Singh, MK Singh, MC Kenney, MJ Jager, MA Rizvi, R Meel. Prognostic significance of PD-1/PD-L1 expression in uveal melanoma: Correlation with tumor-infiltrating lymphocytes and clinicopathological parameters. Cancer Immunol Immunother 2021. [Google Scholar]
- C Robert, G V Long, B Brady, C Dutriaux, M Maio, L Mortier. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 2015. [Google Scholar]
- K Namikawa, A Takahashi, T Mori, A Tsutsumida, S Suzuki, N Motoi. Nivolumab for patients with metastatic uveal melanoma previously untreated with ipilimumab: A single-institution retrospective study. Melanoma Res 2020. [Google Scholar]
- JJ Bosch. Immunotherapy of uveal melanoma. Dev Ophthalmol 2012. [Google Scholar]
- JJ Bosch, UK Iheagwara, S Reid, MK Srivastava, J Wolf, M Lotem. Uveal melanoma cell-based vaccines express MHC II molecules that traffic via the endocytic and secretory pathways and activate CD8+ cytotoxic, tumor-specific T cells. Cancer Immunol Immunother 2010. [Google Scholar]
- RD Carvajal, P Nathan, JJ Sacco, M Orloff, LF Hernandez-Aya, J Yang. Phase I Study of Safety, Tolerability, and Efficacy of Tebentafusp Using a Step-Up Dosing Regimen and Expansion in Patients With Metastatic Uveal Melanoma. J Clin Oncol 2022. [Google Scholar]
- K Bilmin, KJ Synkradzkj, AM Czarnecka. New Perspectives for Eye-Sparing Treatment Strategies in Primary Uveal Melanoma. Cancers ( Basel) 2021. [Google Scholar] [Crossref]
- AD Singh. Light activated therapy of choroidal melanoma. A new modality could be an effective alternative to radiation. Retin Physician 2019. [Google Scholar]
How to Cite This Article
Vancouver
Maurya RP, Nahid Z. Recent advances in the management of uveal melanoma [Internet]. IP Int J Ocul Oncol Oculoplasty. 2024 [cited 2025 Sep 10];10(3):114-116. Available from: https://doi.org/10.18231/j.ijooo.2024.023
APA
Maurya, R. P., Nahid, Z. (2024). Recent advances in the management of uveal melanoma. IP Int J Ocul Oncol Oculoplasty, 10(3), 114-116. https://doi.org/10.18231/j.ijooo.2024.023
MLA
Maurya, Rajendra P, Nahid, Zainab. "Recent advances in the management of uveal melanoma." IP Int J Ocul Oncol Oculoplasty, vol. 10, no. 3, 2024, pp. 114-116. https://doi.org/10.18231/j.ijooo.2024.023
Chicago
Maurya, R. P., Nahid, Z.. "Recent advances in the management of uveal melanoma." IP Int J Ocul Oncol Oculoplasty 10, no. 3 (2024): 114-116. https://doi.org/10.18231/j.ijooo.2024.023
