Introduction
Ptosis is defined as droopiness of the upper eyelid.1 It can be broadly classified as congenital or acquired. Congenital ptosis occurs due to a developmental dystrophy of the levator muscle. Acquired ptosis can be further classified into neurogenic, myogenic, traumatic, and mechanical. 2 Upper 2 mm of cornea is normally covered by upper eyelid and is implicated in inducing static pressure on the ocular surface. The induced pressure on cornea results in it assuming the typical with-the-rule astigmatic shape. 3, 4 Lower-placed upper eyelid in ptosis may lead to significant refractive errors, corneal surface topographic changes and induced astigmatism. 5, 6 The asymmetric and irregular topographic changes are noted in congenital ptosis and they lead to clinically significant astigmatism. 5 In fact, the most common refractive error seen in ptosis is astigmatism. 6, 7 The increased prevalence of with-the-rule (WTR) astigmatism seen in eyes with ptosis supports this hypothesis. 8 This is the first study of its kind to author’s knowledge which studied both refractive errors and corneal topographic changes and tried to estimate their prevalence in Indian population in congenital ptosis cases. On assumption that eyelid pressure leads to the development of significant changes in corneal surface and refractive errors, this study was undertaken with primary objective to estimate the prevalence of errors of refraction and corneal surface (topographic) changes in congenital ptosis. The secondary objective was to study the relation between severity of ptosis and occurrence of corneal topographic changes and refractive errors.
Materials and Methods
This was a cross-sectional analytical observational study conducted from Jul 2021 to Feb 2023 at Nav Jyoti Eye Hospital (a super-specialty eye hospital), Gorakhpur, Uttar Pradesh.
Inclusion criteria
The study included patients of unilateral simple congenital ptosis seen in outpatient clinics of eye hospital. 83 subjects satisfied the inclusion criteria and were enrolled.
Exclusion criteria
All cases of ptosis other than simple congenital ptosis like myogenic, aponeurotic or senile ptosis were excluded. Also, subjects with vision abnormalities due to cataract, glaucoma, corneal opacities, previous history of ocular surgery and patients unwilling to give consent were also excluded from the study. 27 subjects were excluded.
Sample size calculation
The sample size was calculated to test the hypothesis H0: μ1 – μ2 =0 against H1: μ1 -μ2 ≠ 0 when μ1 and μ2 are proportion values of a study variable in eyes with congenital unilateral ptosis (Group 1) and fellow eye (Group 2) respectively. The formula used for sampling was:
The sample size was calculated using prevalence of refractive errors (astigmatism > 1D and spherical equivalent > 1D) in ptotic eyes as 37.04%5 and that in normal eyes as 18% (values taken from previous study). 5 5% significance level and 80 % power were used to calculate sample size. Optimal sample size found was 83. Ethical clearance was taken from institutional review committee of NavJyoti Eye Hospital and Laser Centre on 05 Jul 21 with reference number 010721 and data collection was started on 15 Jul 21. The written informed consent was obtained from all study participants.
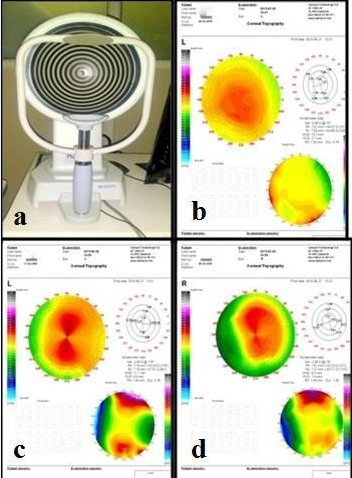
All participants were evaluated by the same doctor. Visual acuity by Snellen’s chart was taken for children >5 yrs of age whereas Picture chart or Tumbling E-charts were used to obtain visual acuity for children <5 yrs of age. A comprehensive slit lamp and fundus examination were performed. Ptosis was evaluated to measure margin reflex distance 1 and 2 (MRD1 and MRD 2), Margin limbal distance (MLD). Levator Palpebrae Superioris (LPS) Function was measured by using ruler and torchlight. Ointment Atropine 1% BD for 3 days was given to younger children of < 5years of age and they were evaluated on the fourth day. Subjects > 5years of age were evaluated on the same day of visit post dilatation with cyclopentolate 1% 3-4 times every 15 minutes. Same doctor did retinoscopic refraction for all participants and was recorded in spherical equivalent (SE) notation. Placido disc based corneal topographer PCT-200 by Optopol (Figure 1) was used to obtain Sim K values and astigmatism. Astigmatism from topography was labelled as Sim K astigmatism. Sim K gives the power and location of the steepest meridian and the meridian 900 away.5
The configuration of the predominant pattern seen on the map was used to classify corneal topographs and five types of corneal topographic patterns were labelled: round, oval, symmetric bow tie, asymmetric bow tie and irregular as described by Bogan SJ et al.9
SE was obtained by using formula [SE = Spherical value + [cylindrical value /2] (in dioptres)]. SE of ≤ -0.5D was labelled as myopia, SE ≥ +1 D as Hyperopia and astigmatism of only ≥ 1 D was considered significant. 10, 11 Cylinder values obtained from retinoscopy was labelled as refractive astigmatism. The distance in mm from corneal light reflex to the upper lid margin with subject’s eye in the primary position of gaze was taken as MRD 1. In cases of non-visible reflex, the eyelid was raised till corneal light reflex visible and value was recorded as a negative number in mm. Normal MRD1 is 4 to 5 mm. 2 Classification of ptosis was done as per MRD 1 12 values as mild if between 4 to 2 mm, moderate if 1 mm and severe if ≤ 0mm [Table 1].
Statistical analysis
Data was analysed using SPSS (Statistical package for social sciences) version 20.0. Proportions of refractive errors and corneal topographic changes in ptotic and non-ptotic groups were compared using Chi-square test or 2 independent sample t-test while mean astigmatism in various degrees of ptosis was compared by Fisher’s test or ANOVA test. Significant P-value taken was < 0.05.
Results
83 eyes of 83 subjects with unilateral simple congenital ptosis were included in the study. 83 fellow non-ptotic eyes were studied for comparative analysis. The sex distribution in study subjects was equal with 42 (50.60%) males & 41 (49.40%) females. Most of the subjects were <30 years of age with mean age being 16.52 ± 12.59 years [Table 2]. Keeping in mind the primary objective of estimation of prevalence of refractive errors and corneal topographic changes in congenital ptosis and secondary objective of study of relation between severity of ptosis and occurrence of corneal topographic changes and refractive errors, the findings were analyzed. By using chi-square test, it was seen that there was significant difference in visual acuities in ptosis and non-ptosis group where ptotic eyes were found to have decreased visual acuities (P value < 0.001) [Table 3]. Of 83 eyes with ptosis, 51 (61.45 %) had visual acuity (VA) of ≥ 6/12, 23 (27.71 %) had VA of 6/18 - 6/36 and 9 (10.84 %) had VA of ≤ 6/60. Similarly, 71 (85.54 %) of normal eyes had VA of ≥ 6/12, 5 (6.02 %) had VA of 6/18 - 6/36 and 7 (8.44 %) had VA of ≤ 6/60.
Of 83 subjects, 18 (21.69%) had mild ptosis, 30 (36.14 %) had moderate ptosis while 35 (42.17%) had severe ptosis. The association between reduced visual acuity and severity of ptosis was found to be significant. [VA of ≤ 6/60 was seen in 2 eyes with mild ptosis, 4 eyes with moderate and 3 eyes with severe ptosis while 7 of normal eyes had VA of ≤ 6/60] More severe ptosis subjects had poorer visual acuities (Fisher’s test, P-value=0.001) [Table 4].
Refractive errors
Of 83 ptotic eyes, 16 (19.28%) had myopia and 14 (16.86%) had hyperopia and 38 (45.78%) had astigmatism. The prevalence of these refractive errors was significantly more in ptotic eyes as non-ptotic eyes [10 normal eyes (12.05%) myopic and 2 eyes (2.41%) hyperopic] (Chi-square test, P value = 0.001) [Table 3].
The ptotic eyes had mean refractive astigmatism of 0.880 ± 0.662 D while same in non-ptotic eyes was 0.449 ± 0.602 D. The prevalence of refractive astigmatism was significantly more in ptosis group with 38 ptotic eyes (45.78%) having astigmatism as compared to 5 (6.02%) non-ptotic eyes (2 independent t-test, P value < 0.001) [Table 3]. There was positive association between severity of ptosis and astigmatism. Prevalence of astigmatism increased with increase in severity of ptosis (ANOVA test, P value < 0.001) [Table 4].
Table 1
Grading of ptosis based on MRD 1: 12
|
Grade of Ptosis |
Drooping of Upper eyelid from normal position |
MRD 1 |
|
No Ptosis |
0 |
>2 |
|
Mild |
Upto 2 mm |
2 |
|
Moderate |
3 mm |
1 |
|
Severe |
≥ 4 mm |
≤0 |
Table 2
Demographic characteristics of study participants
|
Characteristic |
|
|
Patients |
83 |
|
Age (years), Mean±SD |
16.52 ± 12.59 |
|
Sex, M:F ratio |
1.02:1 |
|
Ptosis Severity distribution (%) |
|
|
Mild |
18 (21.69%) |
|
Moderate |
30 (36.14 %) |
|
Severe |
35 (42.17%) |
Table 3
Summary of clinical, refractive and corneal topographic findings in ptotic eyes and its comparison with normal fellow eyes
Table 4
Distribution of refractive and corneal topographic parameters with respect to the severity of ptosis
Figure 1
Corneal topography. a: Placido disc based corneal topographer PCT-200 by Optopol and; b,c,d: Topography maps showing round, symmetric bow tie and asymmetric bow tie patterns respectively.
Of 38 ptotic eyes with significant astigmatism, 08 had myopia ≥ -0.5D and 10 had hyperopia ≥ +1 D. Therefore, 50 out of 83 ptotic eyes had refractive errors (16 eyes with myopia, 14 eyes with hyperopia and 20 eyes with astigmatism). The actual prevalence of refractive errors in ptotic eyes was 50 (60.24%) while 33 (39.76%) eyes were emmetropic. Of 38 ptotic eyes with significant astigmatism, 20 were having myopic astigmatism, 13 had hyperopic astigmatism and five had mixed astigmatism. 14 (16.87%) of non-ptotic eyes had refractive errors [out of 5 normal fellow eyes having significant astigmatism, 2 had myopia ≥ -0.5D and 1 had hyperopia ≥ +1 D]. The ptotic eyes had mean Sim K astigmatism of 1.278 ± 0.656 D while same in non-ptotic eyes was 0.871 ± 0.426 D. Significant sim K astigmatism was found more in ptotic eyes [48 (57.83%)] as compared to 24 (28.92%) non-ptotic eyes (2 independent t-test, P value < 0.001) [Table 3].
Corneal topographic patterns
We found that most of the ptotic eyes [44 (53.01%)] showed symmetric bow tie pattern on topography while non-ptotic eyes had round pattern (39.76%) as the most common pattern. The occurrence of bow tie pattern was significantly more in ptotic eyes (66.26%) vs non-ptotic eyes (32.53%). 20 ptotic eyes (24.09%) showed round and oval pattern while 53 non-ptotic eyes (63.86%) had round and oval pattern [Table 3]. The increased severity of ptosis was associated positively with increased occurrence of bow tie pattern. A significant association was seen between distribution of topographic patterns and severity of ptosis (Fisher’s test, P value < 0.001) [Table 4].
Discussion
We found equal distribution of ptosis in males and females which was similar to the study by PV NK et al which had 56% males and 44% females. 6 Present study had 91.57% subjects under 30 years of age and 63.85% subjects under 20 years of age. Similar age distribution was reported by PV NK et al with 67.27% patients < 20 years 6. Similarly, Bavishi AK reported 51% subjects were between 11 to 20 years of age. 13 The present study found mean age of the subjects as 16.52 ± 12.59 years which was similar to the study by Huo L et al on form deprivation amblyopia in unilateral congenital ptosis in which mean age of patients was 16.83 years. 14 We found relatively higher prevalence of severe ptosis in our study (42.17%) compared to other studies in literature reporting lower incidence. 14 This finding may be because of decreased awareness and late presentation to eye care facilities in our population.
We noted poorer visual acuities in ptotic eyes and it may be due to the occurrence of more refractive errors in ptosis. The finding of association between decreased visual acuity and increase in the severity of ptosis seen in our study was similar to the study by DA Kumar et al who found that severe ptosis group with low MRD had poor vision. 15 Thapa R found that 25% subjects of congenital ptosis had visual acuities less than 6/18. 7 The different inclusion and exclusion criteria could be the reason for finding of more eyes with visual acuity <6/18 in our study.
We found more prevalence of myopia and hyperopia in ptotic eyes than in non-ptotic eyes. This finding substantiates the similar findings reported by various studies with occurrence of higher prevalence of refractive errors in ptotic eyes. 6, 7, 16 We found that frequency of refractive errors (myopia and hyperopia) increased with severity of ptosis where 25% myopic eyes had moderate ptosis and 37.5% myopic eyes had severe ptosis. Similarly, 35.71% hyperopic eyes had moderate ptosis and 64.29% had severe ptosis.
We used two methods to estimate the prevalence of astigmatism viz cycloplegic retinoscopy and corneal topography. Retinoscopic astigmatism was significantly more in ptotic eyes as compared to non-ptotic eyes. Similar findings were reported by Ugurbas and Zilelioglu where they found significant astigmatism in 33% ptotic eyes vs. 6% in control group. 5 Similarly, Huo L et al also reported high prevalence of astigmatism in ptotic eyes. 14 The review of available literature shows prevalence of astigmatism in ptotic eyes ranging from 8.9% as reported by Thapa R to 32.4% as reported by Hashemi H et al. 7, 17 However, the criteria used to define astigmatism vary in different studies. Few studies considered it significant if ≥ 0.5D while some took it significant if it is ≥ 1D. 10, 11, 18 Huo L et al defined > 0.75D as astigmatism while Paik Ji-Sun et al considered amblyogenic astigmatism as ≤ 1.5 D and they substantiated finding of more prevalence of refractive astigmatism (47.76%) in ptotic eyes. 14, 12 Astigmatism by topography also revealed similar findings. In this study astigmatism was found to be positively associated with severity of ptosis which is similar to study by CONGÉNITA EN et al who reported more likelihood of having astigmatism with severe ptosis. 8
The ptotic eyes in this study had symmetric bow tie as most common pattern on topography and its frequency increased with severity of ptosis. The corneal topographic patterns seen in our study are similar to the study by Ugurbas and Zilelioglu which concluded that incidence of bow tie pattern was significantly more in ptotic eyes (55.56%). 5 We found higher prevalence of clinically significant astigmatism in ptotic eyes was in accordance with the most commonly observed topographic pattern i.e. symmetric bow tie pattern. Our study concluded that eyelid ptosis has a pernicious effect on topography which becomes more asymmetrical and irregular (08 ptotic eyes had an irregular pattern as compared to 03 non-ptotic eyes). We found that the prevalence of topographic astigmatism (57.83%) was more than retinoscopic astigmatism (45.78%) in ptotic eyes which may be because topography could detect astigmatism earlier than it is detectable clinically by refraction.
The limitation of this study was that it was an observational study with inclusion of only simple congenital ptosis cases. Ptosis can be co-existent with pre-existing refractive errors and corneal topographic patterns. So, further prospective experimental studies are needed to substantiate the findings of this study. However, it could be inferred from present study that the detrimental effects of eyelid ptosis on the cornea and refractive status of the eye could be detected earlier with corneal topography. Hence, authors recommend that meticulous refraction and corneal topography should be done in all congenital ptosis cases to timely detect astigmatism and suitable corrective measures should be instituted to prevent the development of amblyopia.
Conclusion
Significant refractive errors and corneal topographic changes are seen in congenital ptosis when compared with non-ptotic eyes. The most common refractive error seen in ptotic eyes is astigmatism. The greater prevalence of topographic astigmatism (57.83%) than retinoscopic astigmatism (45.78%) underlines the need of corneal topography in all ptosis patients to ensure detection of astigmatism in time and corrective measures institution to prevent development of amblyopia.
