Introduction
Conjunctival chemosis, the collection of excess fluid in conjunctiva is a common ophthalmic finding with varying severity, symptoms, signs and underlying pathology. Though most are ocular in origin either due to allergy, infection or irritation it can also occur as a part of systemic diseases. Features like periorbital edema, proptosis, corkscrew conjunctival vessels etc. point towards systemic causes. It is important to recognize the underlying cause of chemosis for timely management.1
Case Presentation
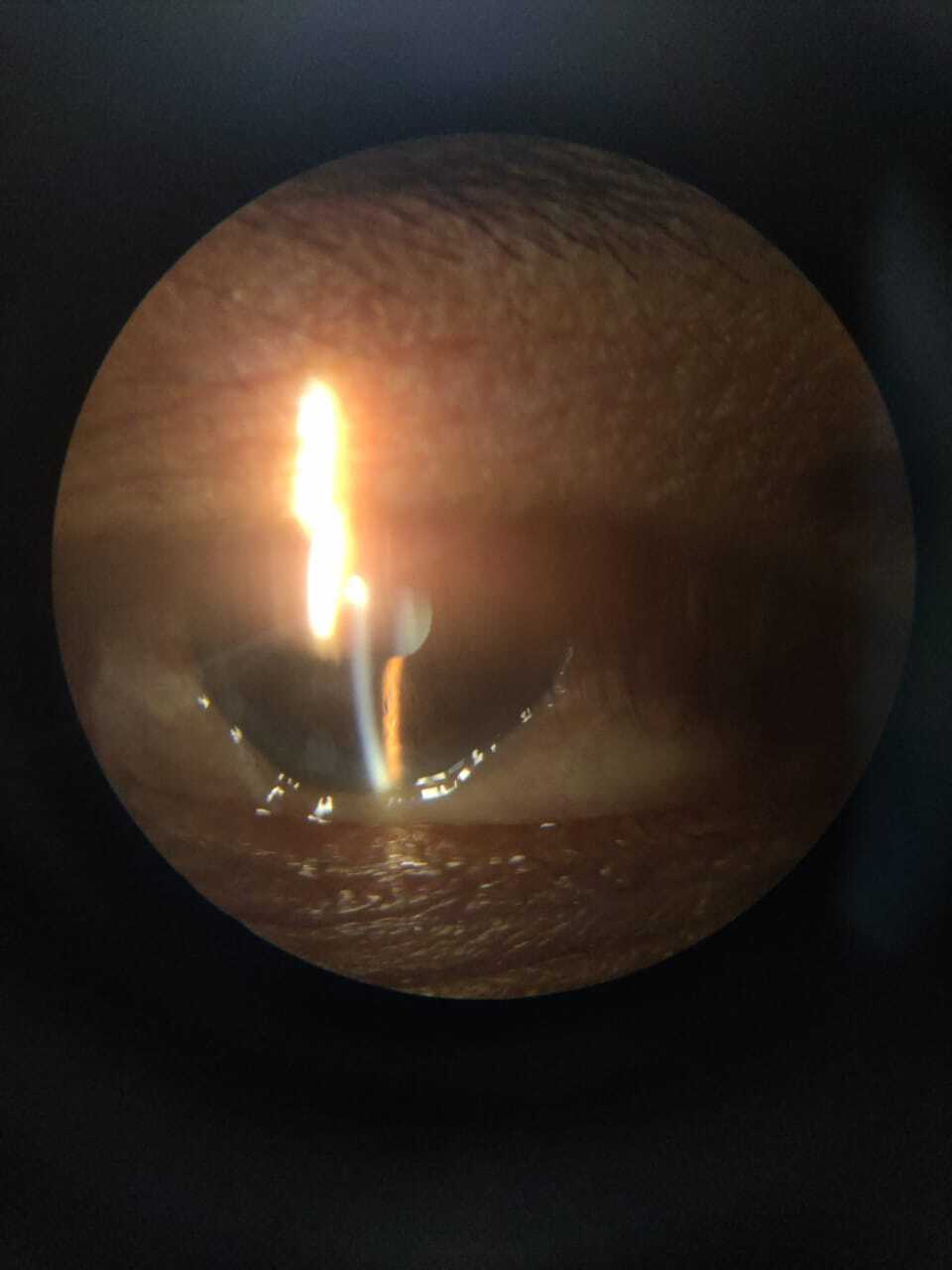
We report a case of a 53-year-old man came to Ophthalmology out patient department complaining of irritation in both eyes for the last two months. There was no history of blurring of vision / head ache/ loss of weight or loss of appetite. Patient had no other comorbidities. General examination revealed facial puffiness, dilated veins over neck and pedal oedema [Figure 1]. His blood pressure (BP) was 140/80 mm Hg and pulse rate was 72 per minute. On ocular examination, best corrected visual acuity (BCVA) was 6/12 in both eyes (BE). He had mild periorbital oedema and chemosis in both eyes. [Figure 2]. Fundus was normal except for mild macular oedema (BE). Intraocular pressure (IOP) was 22 mm mercury (Hg) in both eyes. Gonioscopy showed blood in Schlemm’s canal in all quadrants bilaterally. Optical coherence tomography (OCT) showed minimal fluid collection at the macula. B scan was normal. These features were suggestive of elevated episcleral venous pressure bilaterally.
Medicine consultation was done to find out the cause for this increased venous pressure. Clinical diagnosis of superior vena caval (SVC) obstruction was made, which was confirmed by computerised tomography (CT) neck and thorax. CT revealed features like mild prominence of right internal jugular vein (IJV) [Figure 3], multiple scattered soft tissue density nodes in both lungs and a calcified nodule in superior segment of left lower lobe, possibly metastatic nodule [Figure 4]. Heterogeneously enhancing soft tissue density with focal calcification was noted in left suprarenal region suspicious of malignant adrenal carcinoma. [Figure 5]
Figure 3
Cross sectional CECT imaging at the level of neck shows no obvious focal lesions however Right Iinternal Jugular Vein shows mild prominence

Figure 4
Cross sectional CT thorax images show multiple varying sized soft tissue density nodular lesions scattered in bilateral lung fields suggestive of metastatic nodules
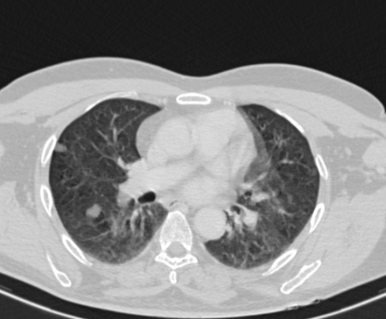
Figure 5
Cross sectional CT imaging at the level of adrenal gland shows large lobulated heterogeneously enhancing soft tissue density lesion with calcific foci in the suprarenal location

Pulmonology and Oncology consultations were also done and an enlarged left supraclavicular lymph node was detected. Patient underwent positron emission tomography (PET) scan and cervical lymph node biopsy.
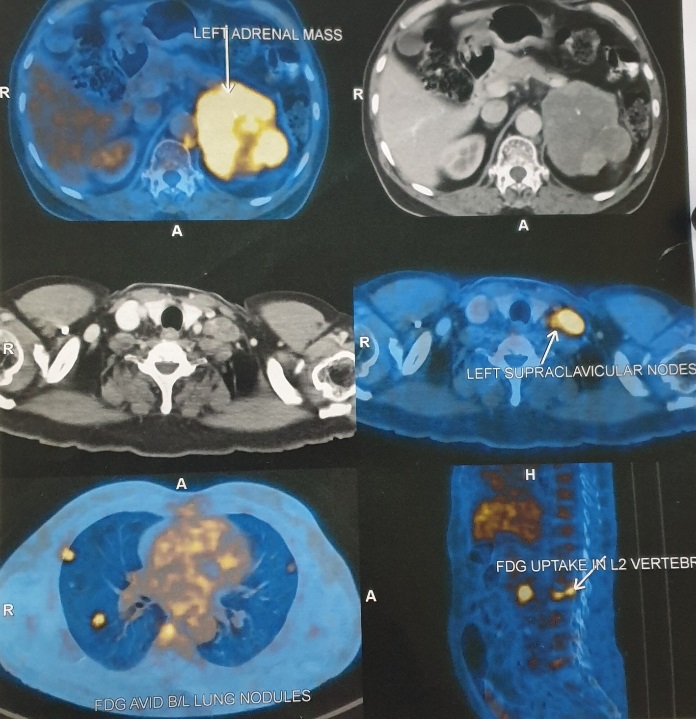
PET scan revealed flurodeoxyglucose (FDG) avid large lobulated soft tissue mass with necrotic areas replacing left adrenal gland, measuring 82×78×74 mm closely abutting left diaphragmatic crura and inferior pole of spleen with loss of fat plane. The lesion pushed the distal body and tail of pancreas anteriorly. These features were suggestive of primary left adrenal malignancy. It also revealed FDG avid discrete and conglomerate multiple enlarged cervical lymph nodes, highest mediastinal nodes, abdominal, para aortic, preaortic and retrocrural lymph nodes. Soft tissue nodules were noted in bilateral lung fields, degenerative partial wedge compression in L2 vertebra, focal pyelonephritis and suspicious renal cortical neoplasm [Figure 6]
Figure 6
This image shows PET scan with increased upatake in left adrenal gland, bilateral lung nodules , left supraclavicular lymph node and L2 vertebrae
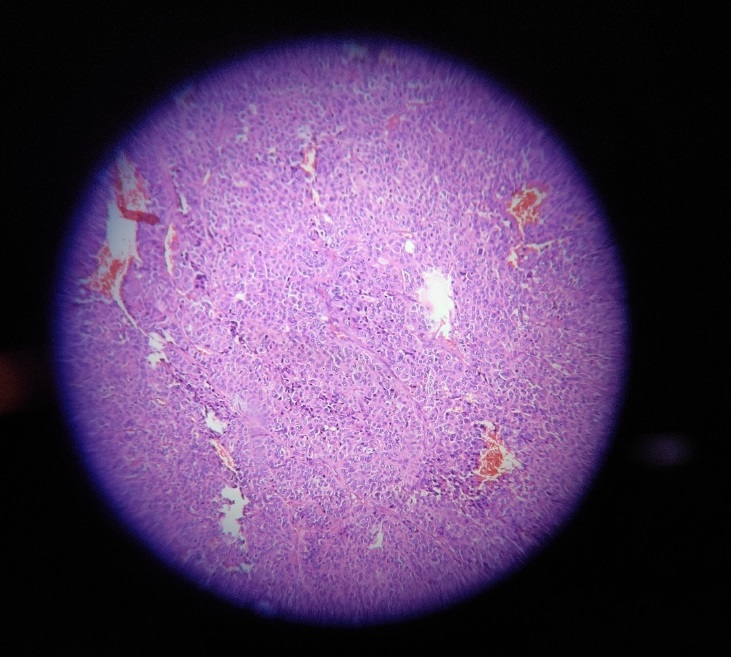
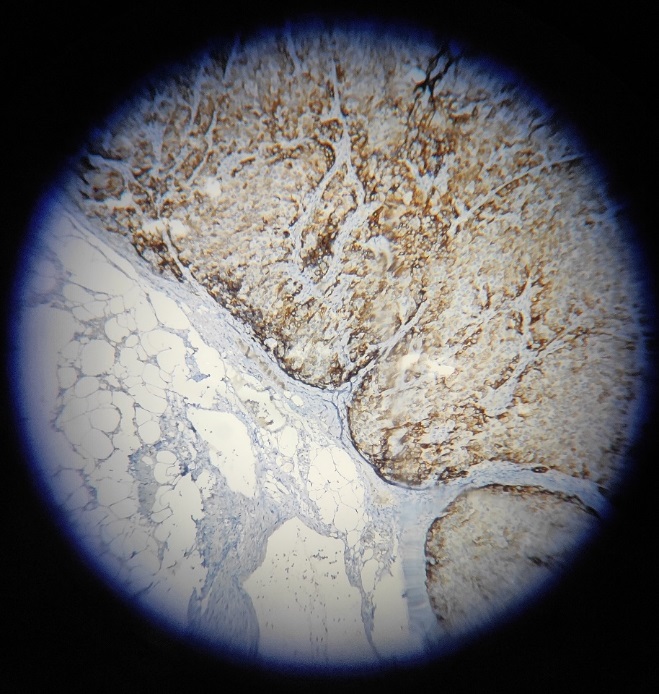
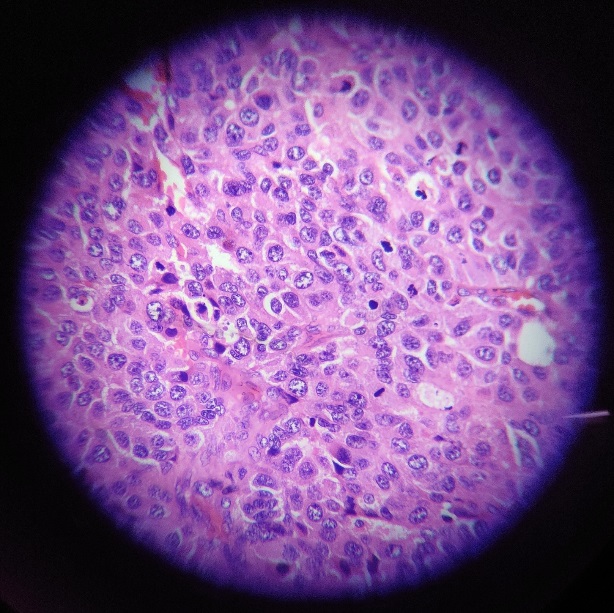
The cervical lymph node biopsy confirmed metastasis from poorly differentiated carcinoma possibly adrenocortical carcinoma. It showed complete effacement of architecture, showing a neoplasm composed of cells arranged in nests and sheets. Individual cells had moderately eosinophilic/ clear cytoplasm and pleomorphic vesicular nucleus with prominent nucleoli [Figure 7]. Mitosis were noted 6-7/high power field(hpf). Multiple areas of haemorrhages were present [Figure 8]. IHC was done and tumour cells were inhibin and synaptophysin positive [Figure 9]. Other markers like p63, thyroid transcription factor (TTF1), napsin, melanin A were negative.
Figure 7
Cervical lymph node biopsy 40x shows complete effacement of architecture, composed of cells arranged in nests, individual cells moderately eosinophilic, clear cytoplasm,pleomorphic vesicular nucleus,high mitosis 6-7/hpf
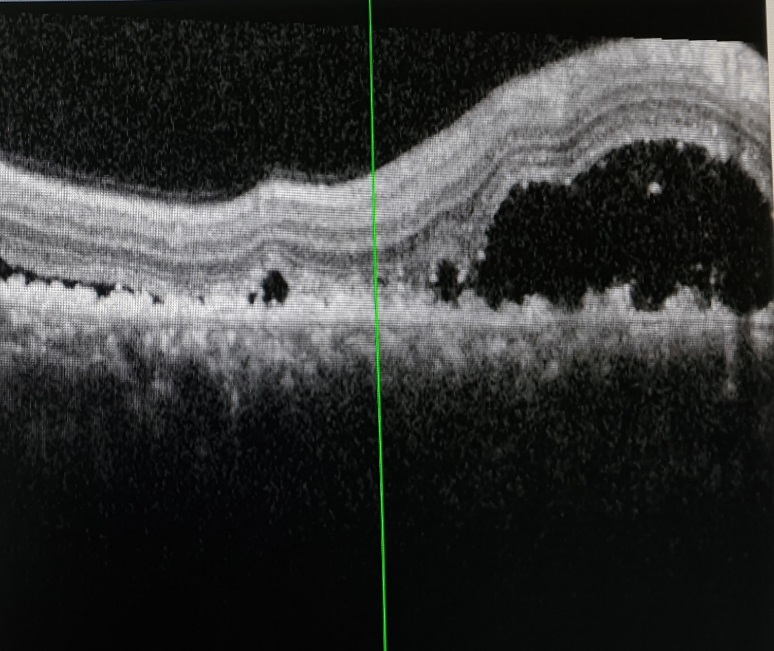
During follow up visit in our department, patient had further deterioration. His BCVA worsened to 6/36 BE. There was persistent chemosis BE and dilated and tortuous episcleral vessels. IOP was under control with topical timolol eye drops. Fundus showed increased fluid collection in all quadrants with shifting fluid. OCT showed increase in central foveal thickness (CFT) and peripapillary fluid [Figure 10].
Unfortunately, patient expired after 1 month, due to brain metastasis and brainstem bleed.
Discussion
Bilateral chemosis is often a reversible clinical finding, resulting from local or systemic causes. In the presence of persistent bilateral chemosis, systemic causes should be ruled out.
Common ocular etiologies of conjunctival chemosis are inflammations like conjunctivitis (either infective or allergic), scleritis, episcleritis and orbital diseases like orbital cellulitis. Conjunctival desiccation by ocular surface exposure is one of the major causes of conjunctival chemosis.
Systemic causes include acute allergic reaction to food or drugs, carotid cavernous fistula (CCF), Superior vena cava syndrome, various malignancies, cardiac, renal and pulmonary diseases, fluid overload, hyperthyroidism etc.
Chemosis along with dilated episcleral vessels and blood in Schlemm’s canal aroused the suspicion of elevated episcleral venous pressure, the important causes being arteriovenous malformations such as CCF, orbital varices, Sturge-Weber syndrome, and conditions that lead to venous obstruction such as retrobulbar tumour, thyroid eye disease and SVC syndrome.
The co existing periorbital puffiness and dilated veins over head and neck region, in turn aroused the possibility of SVC obstruction. Further detailed examination led to the discovery of enlarged cervical lymph nodes and final revelation of the basic pathology, which turned out be an occult adrenal malignancy.
Systemic tumours can result in significant ocular symptoms. Extra ocular tumours are primary tumours that originate outside the eyeball, most commonly in the brain, although they can arise in the lung, breast, liver, nasopharynx, and other bodily organs 2 One among them is adrenal metastasis, though it is very rare. A case report of a patient with adrenal adenoma describes cushingoid characteristics, including obesity, face puffiness, and pruritic blue striae. 3 Ocular examination showed exudative retinal detachment (RD) in the RE and pigment epithelial detachment (PED) with peripheral subretinal fluid in the LE suggestive of multifocal central serous retinopathy (CSR) in BE. 3
A similar case was reported as bilateral conjunctival oedema as a symptom of adrenal adenocarcinoma.(4)They reported chemosis in BE which was not improving with antibiotics and anti-inflammatory treatment. After complete systemic examination, patient was diagnosed with adrenocortical carcinoma which was treated by surgery and chemotherapy. Patient symptoms subsequently improved.4 This case scenario is very similar to our case report.
Another case report of pheochromocytoma showed cushingoid features, pain on eye movements and normal ophthalmological examination except for unilateral proptosis.5
Adrenocortical carticnoma (ACC) is a rare malignancy which can affect anyone at any age, with the first peak incidence occurring in the first decade and the second peak occurring between the ages of 40 and 50.In about 50% cases, it runs in families. The majority of affected people (55–60%) are women. It can be functioning and non functioning. Functioning ACC produce excess hormones than it normally should and vice versa. It is associated with certain conditions like Beckwith Wiedemann syndrome, Familial Adenomatous Polyposis (FAP), Li Fraumeni syndrome.6 Exact etiology is not known. Symptoms are mainly due to overproduction of hormones and mass effect in large tumors. Common clinical presentation are abdominal pain, precocious puberty, features of elevated cortisol level like high blood pressure, high blood sugar, weight gain and features of deranged sex hormones. Blood levels of hormones need to be assessed. Increase in cortisol level can lead to conjunctival chemosis and facial puffiness, though in this case, there were features of SVC obstruction due to enlarged cervical lymph nodes. Imaging modalities like CT, PET scan and tissue biopsy help in diagnosis.
Treatment modalities include surgery, radiation, chemotherapy and immunotherapy. Overall, the prognosis of patients with ACC is poor. A recent Danish study on 160 patients with ACC showed that a median survival of patients with ACC was 35 months7 whereas in the study based on the USA SEER database, the median survival of patients with ACC was 17 months.8