Introduction
Orbital Apex Disorders comprise orbital apex syndrome (OAS), superior orbital fissure syndrome (SOFS), and cavernous sinus thrombosis (CSS). Orbital apex syndrome (OAS) is also known as Jacod syndrome. OAS is a rare disorder that resulted from the involvement of various structures in the region of the orbital apex by a disease process.1, 2 OAS is presented with proptosis, ophthalmoplegia, and ptosis due to oculomotor, trochlear, and abducens cranial nerve palsies; hypoesthesia can occur along the area of the distribution of the ophthalmic division (V1) of the trigeminal nerve; and visual loss from the optic neuropathy.1, 3, 4
Due to anatomical proximity, two other syndromes that can have overlapping features are the Superior orbital fissure syndrome and the cavernous sinus syndrome.
The term superior orbital fissure syndrome (SOFS) or Rochon–Duvigneaud syndrome is often applied to a lesion located immediately anterior to the orbital apex, including the structures exiting the annulus of Zinn and often those external to the annulus.5 In this clinical setting, multiple cranial nerve palsies may be seen in the absence of optic nerve pathology. CSS is usually present with hypoesthesia of the cheek, and lower eyelid associated with features that occurred in orbital apex syndrome (OAS) due to the involvement of maxillary (V2) division of the trigeminal nerve. CSS may also present with oculosympathetic paresis (Horner’s syndrome) because of sympathetic chain involvement near to internal carotid artery (ICA).1, 6, 7 Our study attempted to give updated information on the advancement of diagnosis facilities and recent management options for OAS.
Clinical Anatomy
The orbital apex is the most posterior part of the orbit positioned at the craniofacial junction. The bone orbital apex is formed by the optic canal and the superior orbital fissure. The optic canal is situated in the superomedial aspect of the OA, and the structures including the optic nerve and ophthalmic artery are passing through it. The SOF is a pear-shaped bony cleft in the orbital apex and located inferolateral aspect to the optic canal with an optic strut that separates it from the optic canal between the roof and the lateral wall of the orbit. [8.13] The SOF has related anteriorly to the annulus of Zinn (common tendinous ring) on which the four rectus muscles attach. The annulus of Zinn divides the superior orbital fissure into three parts: lateral, middle (oculomotor foramen), and inferior. The lateral portions contain the SOV, the trochlear, frontal, and lacrimal nerves. The middle portion of SOF, which is enclosed by the tendinous annulus of Zinn, contains the superior and inferior branches of the oculomotor nerve, the abducens nerve, and the nasociliary nerve. The inferior portions contain the inferior branch of the ophthalmic vein.8, 9, 10 Cavernous sinus is posterior to SOF. The internal carotid artery (ICA) and adjacent sympathetic fibers pass through the medial part of the cavernous sinus, and the first and second division of the trigeminal nerve, oculomotor and trochlear nerves pass through the lateral wall of the cavernous sinus. Abducens nerve is passing through the cavernous sinus between the internal carotid artery and the lateral wall. 11, 12, 13
Table 1
Orbital Apex syndrome constitutes a syndrome characterized by the involvement of the following cranial nerves (C.N) 1, 2
Etiopathogenesis
A large variety of pathological processes can affect the region of the orbital apex, these may be inflammatory, infectious, neoplastic, iatrogenic/traumatic, or vascular in origin (Table 2).
Table 2
Etiologies of orbital apex syndromes[1.2]
Inflammatory Causes
Multiple Seditious causes for orbital apex syndrome are characterized by the following features. 2
Symptoms have a rapid-fire onset and generally progress over days.
Common symptoms include painful limitation of eye movements and may be associated with signs of optic neuropathy Some of the known causes include ANCA(Anti-neutrophil cytoplasmic antibody) associated vasculitis, which is vulnerable- mediated and tends to have a affinity for small and medium- sized vessels. This group of vasculitis includes 3 conditions that are known to beget orbital apex syndrome. 18
Granulomatosis with polyangiitis (known before as Wegener’s Granulomatosis).
Microscopic polyangiitis.
Churg- Strauss syndrome both the systemic form of Wegener granulomatosis, with pulmonary and renal involvement, and its limited form may involve the cavernous sinus.
Seizures and CSS were reported in a case with antineutrophil cytoplasmic antibody- associated vasculitis in the limited form of Wegener granulomatosis. In this case, enhancing lesions of the cavernous sinus and thickened pachymeninges were observed. 10 Orbital sarcoidosis may be present as a granulomatous inflammatory disease without systemic involvement. Common features include diffuse lacrimal gland infiltration, optic nerve sheath infiltration, extraocular muscle thickening, soft tissue infiltration of the eyelid and periorbital areas, and uveitis. The thin section contrasts enhanced MRI (CEMRI) or CT scan of the orbit with contrast is the modality of the choice. 1, 19 Churg – Strauss syndrome (CSS) may also beget orbital apex syndrome. A case with Churg Strauss Syndrome, having a history of asthma, developed severe headaches, progressive left- sided ophthalmoplegia, and visual loss. Laboratory studies revealed eosinophilia, an elevated erythrocyte sedimentation rate, and an elevated perinuclear antineutrophil cytoplasmic antibody position. MRI showed enhancement involving the left superior orbital fissure, cavernous sinus, and dura of the temporal base. 20 Idiopathic orbital inflammatory Disease (IOID) is generally unilateral in grown-ups and bilateral in children. Dacryoadenitis, myositis, orbital soft tissue, and fat infiltration may occur diffusely. Optic nerve sheath, sclera, and uvea may be involved in the disease process. Tolosa Hunt syndrome (THS) is a common cause of orbital apex syndrome. It presents with painful and limited eye movements and although the exact cause remains unknown, it's believed to be due to an abnormal autoimmune response and granulomatous inflammation affecting the orbital apex and/ or cavernous sinus.21 The workup of a case with suspected THS should include a complete white blood count and distribution, cerebrospinal fluid examination for cytology and microbiological workup, and MRI Brain and orbits with gadolinium contrast which has typical findings. CT reviews of the orbit can also help to identify the structures involved. Oculosympathetic nerve fibers conterminous to the internal carotid artery may also be involved in THS. THS may have a relapsing and remitting course; still, residual neurologic deficiencies may persist after remission. Some authors have suggested that other causative conditions should be barred using blood and cerebrospinal fluid examination and possible biopsy if positive findings are seen on MRI or CT. They recommend that follow- up examinations must also be performed for at least 2 times before the opinion of THS is made. 22 Neuroimaging may not be specific for THS, because meningioma, carcinoma, and sarcoidosis may have identical signal intensities on T1- and T2- weighted MRI. 23 The characteristic point of THS is periorbital pain, frequently described as a" gnawing" or" boring" pain, associated with ocular motor nerves paresis, and generally shows a dramatic response to steroid remedy, with utmost cases demonstrating clinical improvement within 48 – 72 hrs., earliest response to steroids is good with utmost cases showing a drop in seditious signs but can relapse on stopping steroids. This warrants a slow taper of steroids and may require cases to be kept on low- cure steroids to obviate relapses. Other seditious causes and fungal infections must be ruled out before starting steroid remedy in THS. Despite a good response to steroids, THS can relapse 24 and a small percentage of cases may need other immunosuppressive agents in addition to/ succeeding steroid remedy. Thyroid- associated ophthalmopathy frequently enlarges all extraocular muscles anteriorly which leads to a crowded orbital apex with dysthyroid optic neuropathy. It's a serious complication of Graves ophthalmopathy, and the management is complex and needs a multidisciplinary approach. Literature reported that medical orbital relaxation by intravenous methylprednisolone is the first- line treatment. 25 The two possible causes for orbital apex syndrome hypothecated are. 26, 27
Infections
Patients with inadequately controlled diabetes or immunocompromised cases are particularly susceptible to infections. Pseudomonas is known to produce toxins and osteoclastogenic lipopolysaccharides that can beget bone destruction and spread. This contrasts with fungal infections which tend to have an angio- invasive nature.28 Rhino-orbital Mucormycosis may lead to vision threatening orbital apex syndrome (Figure 1, Figure 2). Early opinion and critical treatment are vital to reducing mortality and morbidity. Mucormycosis and Aspergillosis should be suspected in individualities with prepping conditions including diabetes mellitus, drunkenness, hematologic malice, and immunosuppression. 29 A fungal cause should be considered in any case taking immunomodulatory, antineoplastic, or long- term corticosteroid remedy. Although fungal infections of the orbit and paranasal sinuses may present with pain, indigenous tissue incursion and necrosis, and typical radiographic findings, they may also do without pain and in an insidious fashion, making the diagnosis more delicate. Orbital apex syndrome is a rare complication of herpes zoster ophthalmicus and tends to have a affection for immunocompromised cases. 30, 31 The possible pathogenic mechanisms are, 32 • Direct cytopathic effect of the contagion • Immune- intermediated tissue damage • seditious edema causing contraction and ischemia. Cases are presented with unilateral vesicular eruptions, vision loss, ophthalmoplegia, and anisocoria along with signs of keratouveitis. generally, ocular manifestations start 1 – 4 weeks after skin lesions. Treatment includes antivirals. The use of steroids as an add- on remedy is still controversial. Parasitic infections include cysticercosis, which originates from an infestation with the excrescencies of Taenia solium and Taenia saginata.33 Orbital cysticercosis may involve both the intraocular structures and orbit particularly the extraocular muscles. The clinical manifestations are caused substantially by the mass effect of the cyst in the initial period resulting in ocular motility restriction and proptosis and depends primarily on the location of the lesion. The most common spots for infestation are subcutaneous tissue followed by the brain and eye. These lesions may affect the extraocular muscles or infrequently indeed the optic nerve. Acute vision loss in a case of orbital cysticercosis is substantially due to compressive optical neuropathy due to a cystic lesion of extraocular muscle or by direct irruption of the optic nerve or because of contraction from the conterminous cyst in intra conal region.34 But direct optic nerve incursion of cysticercosis is a veritably rare reality. The serological tests used for specific opinion of cysticercosis are indirect hemagglutination, indirect immunofluorescence, and immune electrophoresis similar as ELISA serology is the most sensitive. Flair images in MRI reviews have maximal rates of scolex detection and hence should better be considered as a diagnostic disquisition over ultrasonography (USG) and computed tomography (CT) in orbital cysticercosis and neurocysticercosis. 35, 36 Medical management in the form of oral Albendazole combined with oral steroids is the treatment of choice followed by surgical treatment (cyst excision or orbital decompression) to avoid endless vision loss.
Figure 1
(A & B): MRI of patient having Rhino-orbito-ceribral Mucormycosis showing fungal debri in orbital apex region.
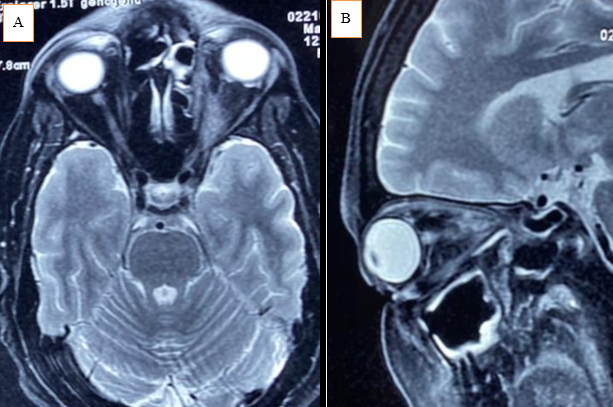
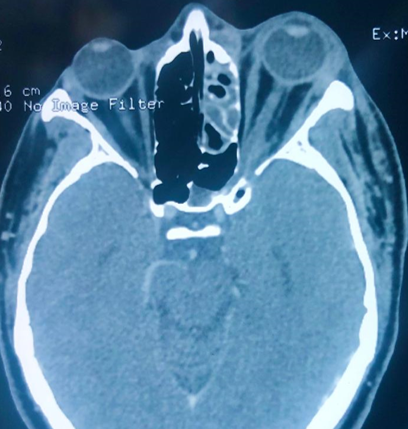
Figure 2
CT-Scan Axial view of patient having Left side Rhino-orbito-ceribral Mucormycosis showing fungal infiltration in left ethmoid sinus and orbital apex leading to proptosis.
Tumors (Neoplasms)
The varied neoplastic causes for orbital apex syndrome include head and neck tumors, hematologic cancers, and metastatic lesions. The varied neoplastic causes for orbital apex syndrome include head and neck excrescences, hematologic cancers, and metastatic lesions. The locoregional spread of head and neck cancers to the draining lymph nodes are the most common spots for metastases with lungs and bones being the most common distant spots. Lymphomatous infiltration of the cavernous sinus has been reported both in pediatric, 35 and adult cases. 37 Carcinoma may be set up in the paranasal sinuses or within the cavernous sinus alone. Neural neoplasms of the orbital apex are most generally benign and include meningiomas, schwannomas, neurofibromas, and, infrequently, ciliary neurinomas. 38 These benign lesions generally result in sluggishly developing orbital symptoms in the absence of pain. Yuen et al(2017) reported a case of a 75- year-old female patient who developed orbital apex syndrome as a presentation of ocular adnexal MALT carcinoma.39 Garala et al(2013) reported a case of an 88- year-old female patient with chronic lymphoid leukemia who developed orbital apex syndrome. 40 Nasopharyngeal rhabdomyosarcomas can also beget orbital apex syndrome in children. 41 Orbital apex pattern can also develop due to compression by neural excrescences in the orbital apex. Meningiomas, schwannomas, and neurofibromas can beget compression of the contents of the orbital apex. A rare case of orbital apex syndrome after initiating treatment of skin carcinoma with Ipilimumab has also been reported.42 Ipilimumab is an IgG1 antibody that targets cytotoxic T lymphocyte- associated protein 4(CTLA- 4). It's known that there are a range of side effects like sterile meningitis, hypophysitis, Guillain- Barre syndrome, transverse myelitis, myasthenia gravis, and symptoms due to gastrointestinal and hepatic system involvement are known. The two possible causes for orbital apex syndrome hypothecated are. 37, 42
Trauma and Iatrogenic Causes
OAS has been observed after both piercing and blunt orbital trauma. 43 piercing trauma leading to OAS is rare in the absence of a bony fracture; still, an OAS has been reported secondary to a retained intraorbital foreign body without bone involvement. Although the delayed onset of neurologic symptoms is rare after an acute traumatic injury, symptoms of a SOFS were delayed for 72 hours in a case with a retained foreign body within the orbit and cavernous sinus. 44 Page 1 of 2 There are reports of trauma resulting in Orbital apex syndrome and generally immediate surgical relaxation of the orbital apex region is needed along with contemporaneous treatment with intravenous steroids. 45 Surgeries for ethmoid artery ligation for intermittent epistaxis, septorhinoplasty, and nasal polyps have been reported to affect in orbital apex syndrome. 46, 47, 48 Jarrahy et al(2001), have reported a case of superior orbital fissure syndrome due to a retained foreign body in the orbit. 49
Vascular Causes
The three main vascular lesions causing orbital apex syndrome are 1, 2, 50
Carotid cavernous fistula (CCF)- these are classified as traumatic or non-traumatic. Traumatic CCFs are most likely due to head trauma and are of the high flow type. Typically, patients present with pulsatile exophthalmos, chemosis, and conjunctival congestion. They can also have raised intraocular pressure due to raised episcleral venous pressure.
Non-traumatic causes lead to low-flow indirect CCFs. These can be seen in patients with hypertension, and patients with Ehler-Danlos syndrome.
CCFs need extensive investigations including ultrasounds, orbital Doppler studies, MRI studies with MRA (Magnetic Resonance Angiography), CT angiography, and catheter angiography, depending upon the individual case the appropriate investigative modality followed by the treatment approach such as conservative management, balloon embolization, and direct or indirect surgery may be considered. 51
Cavernous sinus thrombosis (CST) can be septic or aseptic. Septic causes of CST are seen following infections of paranasal sinuses, orbital cellulitis, tooth, and ear infections. Aseptic causes are seen in hypercoagulable states as in patients on hormone replacement therapy particularly oral contraceptives, pregnancy, malignancies, and congenital causes such as factor V, Leiden mutations, protein C, and protein S mutations. While many carotid cavernous aneurysms may be asymptomatic and relatively "benign" in their course, some aneurysms may grow large enough to cause symptoms due to a mass effect on the adjacent cranial nerves resulting in Orbital apex syndrome like picture. Carotid cavernous aneurysms may also rupture, causing CCF and resultant clinical features.
Other causes
Neurofibromatosis, fibrous dysplasia, and dermoid and epidermoid cysts can also cause orbital apex syndrome.
In type 1 and type 2 Neurofibromatosis, this syndrome may be due to optic nerve gliomas, plexiform neurofibromas, sphenoid wing dysplasia, meningiomas, and schwannomas.
Congenital conditions like fibrous dysplasia can cause orbital apex syndrome by narrowing the optic canal.
Dermoid and epidermoid cysts and mucocele particularly of the ethmoid sinuses can compress the orbital apex. Dermoid cysts in the form of large suprasellar cysts can also lead to cavernous sinus syndrome. A dermoid cyst can rarely rupture spontaneously and lead to inflammation in the surrounding tissues.52 Hence these developmental and congenital conditions cause features of orbital apex syndrome due to mass effect and in rare cases due to inflammation.
Diagnosis and Management
The most common clinical features of a disease process in the orbital apex are vision loss and painful and limited eye movements. Periorbital or facial pain may reflect the involvement of the ophthalmic (V1) or maxillary (V2) branch of the trigeminal nerve. Periorbital pain is one of the diagnostic criteria for Tolosa–Hunt syndrome (THS), an idiopathic inflammatory syndrome of the orbital apex. However, the absence of pain does not exclude a process within the orbital apex. It is important to test the periorbital skin and the corneal reflexes to detect asymmetry in sensation. Involvement of the oculomotor, abducens and trochlear nerves in any combination can lead to ophthalmoplegia and patients can present with vertical, horizontal, or torsional diplopia with or without compensatory abnormal head postures. 1, 2
Other important clinical signs are.
Proptosis
Diplopia
Pupillary abnormalities:
Relative Afferent Pupillary Defect (RAPD) – indicating the involvement of the optic nerve.
Anisocoria – the side of dilated pupil indicating the involvement of the pupillary fibers of the third cranial nerve.
Optic disc edema or optic atrophy
Choroidal folds
Differentiation between cavernous sinus syndrome and orbital apex might be difficult because of the similar involvement of ocular motor nerves and trigeminal nerves; however, the main differentiator is the optic nerve involvement in orbital apex syndrome. This differentiation is important because the etiologies might be significantly different (e.g., Sinus thrombosis for the first versus inflammation or infection).
Neuroimaging is mandatory in patients with orbital apex syndrome. Brain and orbit MRI are the imaging modality of choice and should be performed with gadolinium in case of suspected inflammatory conditions like sarcoidosis, Tolosa Hunt Syndrome, nonspecific orbital inflammatory disease, and vasculitis. MRI with fat suppression sequences is ideal for evaluating the orbital apex and cavernous sinus. Computed tomography (CT) can be done when MRI is contraindicated.1 When a tumor or metastasis is suspected, MRI with gadolinium is recommended to evaluate:
Soft tissue involvement.
Cavernous sinus and intracranial extension.
Bone marrow involvement.
Perineural spread of tumors which are characterized by focal or diffuse thickening of the cranial nerves involved.
In carotid cavernous aneurysms, Magnetic resonance angiography (MRA) or angio-CT scans can be helpful, but angiography remains the gold standard and is useful to plan intravascular treatment. Carotid cavernous fistula can be identified by an angio-CT scan with venous sequences, which can show proptosis, enlarged superior ophthalmic vein, and cavernous sinus. These features can be supported by an MRI with contrast showing a dilated superior ophthalmic vein and post-contrast enhancement of the cavernous sinus. As in an aneurysm, digital subtraction angiography (DSA) is recommended if intervention is being planned. In fractures involving the base of the skull and in those where the zygomaticomaxillary or Naso-ethmoidal regions are involved thin-section CT scans with multiplanar reconstruction are advised. Three-dimensional reconstruction of CT images in such cases can help in planning surgeries. MRI has a limited role in these settings and would only be used for looking at intracranial injuries.
Blood investigations include a complete blood count, erythrocyte sedimentation rate peripheral blood smear, and those directed against a particular infectious agent if suspected should be done. Laboratory testing for inflammation and infection (e.g., erythrocyte sedimentation rate, complete blood count with differential, rapid plasma reagin, micro hemagglutination assay for antibody to Treponema pallidum, angiotensin-converting enzyme, perinuclear antineutrophil cytoplasmic antibody, cytoplasmic antineutrophil cytoplasmic antibody, antinuclear antibody, purified protein derivative, chest radiography, HIV, lumbar puncture) should also be considered if the clinical findings are suggestive of these processes. In inflammatory conditions, the primary option of treatment is with immunomodulatory agents which include corticosteroids and steroid-sparing agents under frequent and close observation of the patient. If vision loss or worsening of ophthalmoplegia is noted on steroids, then repeat imaging should be considered and a biopsy of the lesion also is mandated. 1, 2, 53 Radiation therapy and Orbital decompression may be needed to provide an anatomical expansion of the orbit in dysthyroid optic neuropathy.53, 54 In some cases of Tolosa Hunt syndrome immunosuppressants like methotrexate and azathioprine have been added and in some refractory cases and cases of steroid dependence radiotherapy can be used. 55, 56
The key aspect to remember while dealing with orbital apex syndrome is that treatment is directed toward the underlying condition. The most crucial distinction is between an inflammatory cause and an infection, appropriate broad-spectrum anti-microbial therapy is the treatment of the choice. Fungal infections can worsen very quickly and can be fatal. It is important to exclude fungal infection before initiating steroid treatment.53, 54, 57 In neoplastic cases, Management is dependent on the nature, location, and extent of the lesion. Excision biopsy is the treatment of the choice. Radiation therapy or chemotherapy may be used as adjunct treatment options. 53
In cases of trauma, a CT scan is the gold standard imaging modality and may show comminuted fractures. Corticosteroids can be given for treating orbital compartment syndrome, reducing post-traumatic inflammation and edema, and managing optic nerve injury. Decompressive surgery or definitive orbital wall reconstruction may be done to achieve the aesthetic and functional outcome. While awaiting surgical treatment. 58
Usually, Arterio-venous malformation (AVM) like carotid cavernous fistula (CCF) can be managed conservatively; endovascular or surgical intervention may require for significant cranial nerve dysfunction, associated with raised intraocular pressure. 13, 59 Cavernous sinus thrombosis (CST) requires anticoagulant therapy, corticosteroid therapy may use as an adjunct therapy and aggressive broad-spectrum antimicrobial therapy for the septic causes. An open surgical or endoscopic approach may help drain the pus from an orbital or subperiosteal abscess. 60
Conclusion
OAS represents a heterogeneous group of disorders that result from several etiologies. A systemic disease (i.e., infection, neoplasm, autoimmune condition) may precede the OAS, and a thorough history with a review of systems may offer diagnostic clues; however, an OAS may also be isolated and herald a systemic process. Neuroimaging, preferably with MRI, can confirm the clinical findings of an OAS and identify sites that may be sampled if the diagnosis remains unclear. Treatment is directed at the underlying cause and may require neurosurgical, otolaryngologic, neurologic, or medical consultation. Corticosteroids may be helpful if an inflammatory cause for an OAS is suspected, but should be used judiciously, particularly if an infectious etiology is being considered.
