- Visibility 43 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijooo.2022.012
-
CrossMark
- Citation
A clinical study on prevalence and management of eyelid tumours – A prospective observational study
- Author Details:
-
Malarvizhi R
-
Anuradha A
-
Latha KST
-
Niranjan Karthik Senthil Kumar *
Introduction
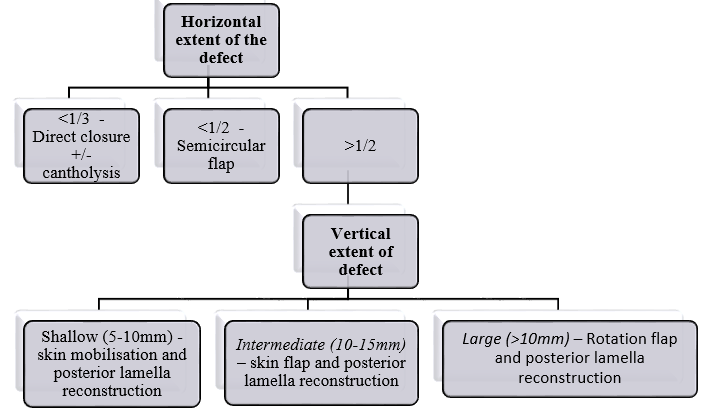
Eyelid lesions are categorised into inflammatory, infectious and neoplastic. Among tumours encountered by ophthalmologist, most common neoplasms are those of eyelids. Lid reconstruction is often essential for tissue loss after wide excision of lid tumors. The process of decision making is mentioned in [Figure 1]. In a study by Jangir et al,[1] the most common benign tumour included epidermal cyst (21.3%), demoid cyst (13.89%), intradermal naevus (12.03%) and haemangioma (12.03%) in western parts of the country. A study by Kaliki et al showed sebaceous gland carcinoma to be most common malignant tumor (53%) followed by basal cell carcinoma (24%) in India.[2] This study is to evaluate the incidence, mode of onset, various clinical presentations of lid tumours. The various treatment options and the final functional and cosmetic outcome of treatment were also assessed.
Materials and Methods
A prospective observational study conducted at Orbit & Oculoplasty Department, Regional Institute of Ophthalmology, Egmore, Chennai for a period of 1 year after obtaining ethical clearance from the institutional ethical committee. All patients with benign and malignant eyelid tumours were included and those with other inflammatory lesions were excluded.
Detailed history including the onset, duration, progression, associated features such as pain, discharge or bleeding from the lesion, site of involvement, history of comorbidities, past history of medical and surgical treatment were noted. Ocular examination including size, shape, location, extent, margins of the ulcer/swelling (specific signs of malignancy i.e. eyelid distortion with thickening of lid in sebaceous cell carcinoma, raised rolled out edges with telangiectasia and ulceration in basal cell carcinoma, induration and everted margins in squamous cell carcinoma) and involvement of adjacent lymph node was done. Blood pressure, blood sugar, complete blood count, X-ray chest and X-ray orbit were performed. For larger lesions or if globe/orbital infiltration is suspected, CT/MRI brain and orbit was done. Biopsy either excision or incision was performed for all the cases and sent for histopathological examination after marking the margins to look for involvement. After HPE confirmation of malignant tumours wide local excision with 4-5 mm margin clearance was done. Defect in the eyelid was reconstructed using appropriate reconstruction procedure. Patients with globe and orbital invasion were referred to tumour board and radical procedure like exenteration was done after getting tumour board clearance. Patients who required adjuvant radiotherapy or chemotherapy were referred to the Department of oncology. All patients were followed up at regular intervals to look for tumour recurrence for 1 year.
Results
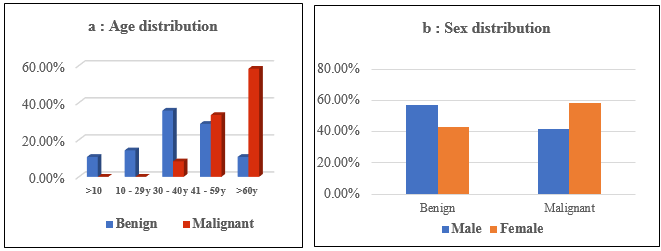
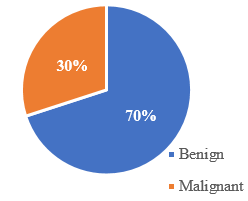
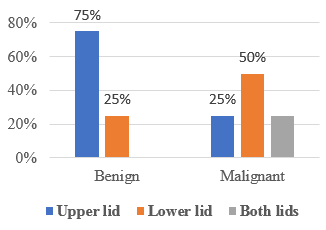
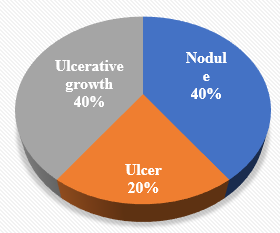
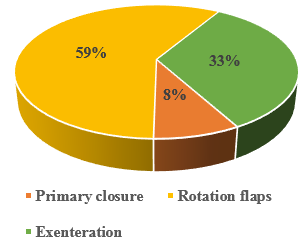
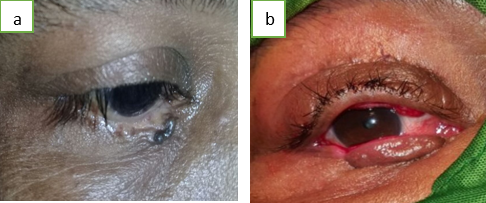
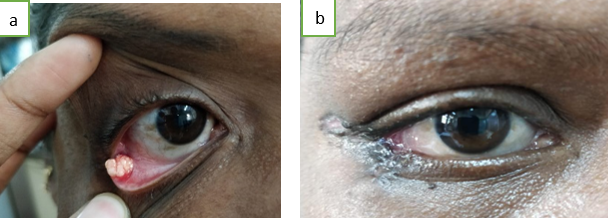
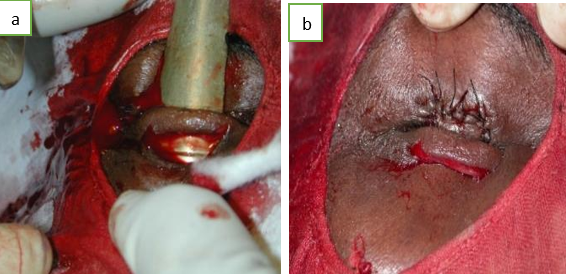
Malignant tumours (7 out of 12 malignancies) were commonly seen in the age group between 60-85 years (58.33%) and benign tumours (7 out of 12 malignancies (10 out of 28 benign tumors) were common in the age group of 30-45 years (35.71%) ([Figure 2]a). Preponderance of benign tumors (57.14%) was observed amng males and malignant tumors (58.33%) preponderance among females ([Figure 2]b). Out of 40 cases, 28 (70%) were benign and 12 (30%) were malignant ([Figure 3]) which correlates with a retrospective study by Sha Sha Yu & Xin Tang.[3] Benign tumours were found more commonly in the upper lid (75%) and malignant tumours in lower lid (75%) ([Figure 4]). Squamous papilloma (7 cases) was found to be the most common benign tumour in this study (25%) ([Figure 5]a) and this was followed by pyogenic granuloma (5 cases - 17.85%). Sebaceous carcinoma (7 out of 12 malignancies i.e. 58.33%) is the most common malignant tumour unlike in the study by Deprez and Uffer [4] which reported that basal cell carcinoma accounted for 86% of all malignant tumors ([Figure 5]b). Most common presentation of malignant eyelid tumours was in the form of ulcerative growth pattern (6 out of 12 malignancies i.e. p50%) ([Figure 6]). In our study both ulcer and nodular pattern is seen in case of BCC. Sebaceous adeno-carcinoma of meibomian gland presented in the form of nodule and ulcerative growth pattern. In our study tumour invasion of the globe was most common in case of sebaceous adenocarcinoma of meibomian gland (3 out of 12 malignant cases i.e. 25%). Lymph node metastasis is most commonly found in sebaceous gland carcinoma (4 out of 7 i.e. 57.14%). The treatment for most of the benign tumour was simple excision and the excised tissue was sent for histopathological examination. In our study one case of capillary hemangioma was managed with systemic and topical beta blockers. The child was started on oral propranolol 1 mg/kg body weight and 0.5% timolol eye drops twice a day after obtaining consensus from paediatrician and cardiologist. Child was reviewed once in three months by ophthalmologist and paediatrician. The lesion started regressing after 4 months of treatment and the treatment was continued with periodic review. Marginal shave excision was done for 5 cases of pyogenic granuloma. In all malignant tumours wide local excision with 4-5mm margins ([Figure 7]). The excised lesion margins are labelled with markers and sutures and sent for histopathological examination. Glabellar rotation flap was performed in one case of meibomian carcinoma involving the medial aspect of lower lid after the excision of the tumour. Hughes tarso-conjunctival flap was performed in two cases of squamous cell carcinoma ([Figure 8]a,b) and basal cell carcinoma, after tumour excision as the defect involved more than 75% of the lower lid without involvement of canthus. Two cases, one each of sebaceous carcinoma and squamous cell carcinoma involving the lateral aspect of lower lid was repaired after excision, with Tenzel lateral advancement flap ([Figure 9]a,b). In one case of sebaceous gland carcinoma with diffuse thickening of whole of the upper lid the tumor was excised and the defect closed with Cutler-Beard technique ([Figure 10]a,b). After 2 months secondary reconstruction was done. One case of basal cell carcinoma managed with tumour excision and Fricke’s flap with chondro-mucosal graft elsewhere reported to us with recurrence of tumour. She was advised exenteration as she presented with orbital infiltration of the tumour. As the patient was not willing for surgery radiotherapy was given as suggested by oncologist. 2 cases of sebaceous cell carcinoma and one case of basal cell carcinoma with orbital infiltration underwent orbital exenteration. One case of advanced sebaceous gland carcinoma who presented to us with infiltration of globe and orbit was advised exenteration as the primary procedure. The patient was not willing for surgery and lost to follow up after that.

Discussion
In our study 40 patients with eyelid lesions were analysed. Out of which 28 patients (70%) had benign and 12 patients (30%) had malignant lesions. This is comparable with a study by Rathod et al [5] where among 100 cases of eyelid tumours 61 were found to be benign and 39 were malignant. Age of the patients with benign lesions were in the range of 30-60yrs and malignant were between 35-80yrs. A case of 36 year old young female patient presented with sebaceous cell carcinoma and 86year old elderly patient was diagnosed with basal cell carcinoma. A study by Kale (2012) et al[6] from India observed that the mean age of presentation of malignant eye tumours was 59 years which is in accordance with our study. In our study, the malignant tumour incidence was more in female patients and benign tumours were most commonly found in male patients. In a study by Gosai et al,[7] 120 cases with eyelid lesions were studied and found that the male to female ratio was 1.4:1 for benign tumours whereas females outnumbered males with ratio of 1.16:1 for malignant tumours which correlated with our study Out of 30% of malignant tumours, Sebaceous gland carcinoma is the most common accounted for 58.33%. Basal cell carcinoma is the second most common accounted for 25%. This is similar to the studies done by Krishnamurthy et al[8] and Mamtani et al[9] which found higher incidence (30-40%) of sebaceous gland carcinoma in India. Among Benign eyelid tumours squamous papilloma is the most common tumour in our study and this is comparable to the studies by Ni et al [10] from China observed that squamous papilloma is the most common benign eyelid tumour. Increased incidence of papilloma was also observed in studies conducted by Gundogan et al[11] and Deprez and Uffer's.[4] The most common presentation of malignant tumours of the upper eyelid was in the form of ulcerative growth. Majority of sebaceous gland carcinoma presented in the form of ulcerative growth and nodule. A study by Syed Ali Raza Rizvi et al[12] found that that most common clinical presentation of SGC was a nodular mass lesion. In this study, the most common site of malignant tumour was lower lid. This corroborates with the studies by A Bagheri et al[13] and Mary Ho et al[14] where they found lower lid to be the most common site of malignant tumours. Studies by Kale et al,[13] Suresh Saquil et al[15] and various other studies have reported greater occurrence of sebaceous cell carcinoma in the upper eyelid. However in our study lower lid was most commonly involved in sebaceous carcinoma. In Basal cell carcinoma, intraocular invasion is rare but orbit involvement may occur. Metastasis is rare in BCC and mortality is also less. In our study there was one case of basal cell carcinoma with orbital involvement and without globe infiltration. Most of the malignant tumours in our study was managed by tumour excision with 5 mm surgical clearance and the full thickness defect was reconstructed with appropriate flap techniques. Standard Surgical Excision (SSE) of tumour free margin of 4 mm recommended for Basal cell carcinoma and for squamous cell carcinoma it is 4 mm to 6 mm. In our study, procedures like Hughes tarso conjunctival flap for lower eyelid defect, Cutler-Beard two stage procedure for upper eyelid defect were performed when the defect was large (> 50% lid involvement). In a study by Gündüz et al,[16] lid sharing procedure was preferred for defects more than 50% and Tenzel flaps for defects between 25 – 50%.
Conclusion
Histopathologic examination of all excised lesion involving the lid must be done as an innocuous looking lesion might be malignant. Early clinical diagnosis of malignant tumours with confirmation by incision biopsy, will aid in complete wide excision of tumour After wide excision of malignant tumour appropriate lid reconstruction technique is done as a primary procedure in all our patients and we could obtain good outcomes with no recurrences. Complete eyelid reconstruction requires through knowledge of several techniques and their range of applicability. The ideal goal of reconstruction is to restore physiological functioning of eyelid with respect to vision, lid closure, mobility and tear drainage and to re-establish anatomic integrity to provide better cosmetic appearance. Advanced tumours with orbital involvement and recurrent tumours will need adjuvant chemotherapy and radiotherapy.
Limitations of the Study
Small sample size and difficulty in follow up.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
None.
References
- M K Jangir, A Kochar, N A Khan, M Jaju. Profile of Eyelid Tumours: Histopathological Examination and Relative Frequency At A Tertiary Centre In North-West Rajasthan. Official Sci J Delhi Ophthalmol Soc 2017. [Google Scholar] [Crossref]
- S Kaliki, N Bothra, K M Bejjanki, A Nayak, G Ramappa, A Mohamed. Malignant Eyelid Tumors in India: A Study of 536 Asian Indian Patients. OOP 2019. [Google Scholar]
- SS Yu, Y Zhao, H Zhao, JY Lin, X Tang. A retrospective study of 2228 cases with eyelid tumors. Int J Ophthalmol 2018. [Google Scholar]
- M Deprez, S Uffer. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. Am J Dermatopathol 2009. [Google Scholar]
- A Rathod, M Pandharpurkar, K Toopalli, S Bele. A clinicopathological study of eyelid tumours and its management at a tertiary eye care centre of Southern India. MRIMS J Health Sci 2015. [Google Scholar] [Crossref]
- S M Kale, S B Patil, N Khare, M Math, A Jain, S Jaiswal. Clinicopathological analysis of eyelid malignancies - A review of 85 cases. Indian J Plast Surg 2012. [Google Scholar]
- J Gosai, D Mehta, K Pherwani, R Bhatt, K Agrawal, D Tandel. Clinical Study of Lid Tumors in Adult Patients of Western Region of India. J Evol Med Dent Sci 2014. [Google Scholar] [Crossref]
- H Krishnamurthy, V Tanushree, HT Venkategowda,, S Archana, G Mobin, A D'Silva. Profile of eyelid tumors at tertiary care institute in Karnataka: a 5-years survey. J Evol Med Dent Sci 2014. [Google Scholar]
- M Mamtani, S Jahagirdar, T Thakre, S Kale, H Kulkarni. A clinicopathological study of eyelid malignancies from central India. Indian J Ophthalmol 2007. [Google Scholar] [Crossref]
- Z Ni. Histopathological classification of 3,510 cases with eyelid tumor. Zhonghua Yan Ke Za Zhi 1996. [Google Scholar]
- F C Gundogan, U Yolcu, A Tas, O F Sahin, S Uzun, H Cermik. Eyelid tumors: clinical data from an eye center in Ankara Turkey. Asian Pac J Cancer Prev 2015. [Google Scholar]
- SA Raza Rizvi, MS Alam, K Akhtar. Eyelid sebaceous gland carcinoma: Varied presentations and reconstruction outcome. Oman J Ophthalmol 2018. [Google Scholar]
- A Bagheri, M Tavakoli, A Kanaani, R B Zavareh, H Esfandiari, M Aletaha. Eyelid masses: a 10-year survey from a tertiary eye hospital in Tehran. Middle East Afr J Ophthalmol 2013. [Google Scholar]
- M Ho, DTL Liu, KKL Chong, HK Ng, DSC Lam. Eyelid tumours and pseudotumours in Hong Kong: a ten-year experience. Hong Kong Med J 2013. [Google Scholar]
- S Sagili, R Malhotra. The importance of considering sebaceous gland carcinoma in presumed chalazia in South Asian patients?. Br J Gen Pract 2013. [Google Scholar] [Crossref]
- K Gündüz, S Demirel, I Günalp, B Polat. Surgical approaches used in the reconstruction of the eyelids after excision of malignant tumors. Ann Ophthalmol (Skokie) 2006. [Google Scholar]
