Introduction
Divided nevus of eyelids is a rare form of melanocytic nevus; which are benign proliferation of melanocytic cells. It presents on both the upper and lower eyelid unilaterally and usually congenital but few cases are reported in literature where it appeared later in life also.1 As this nevus extends up to the lid margins, its edges touch or “kiss” when the eyelids are closed; therefore known as kissing nevus.
It was first described by Fuchs in 1919 and occurs due to a rare embryological phenomenon, therefore only less than 40 cases are reported in literature till date. The kissing nevus origin dates to melanocyte migration or Schwann cells of neuroectodermal origin, during embryological fusion of eyelids at 9th week of gestation and later during the course of fetal development, when the eyelids eventually separate, the single nevus divides into two distinct portions: one on the upper and one on the lower eyelid. 2, 3
The nevi are usually asymptomatic and spare other eye structures, such as conjunctiva, sclera, and cornea. The presenting symptom of eyelid kissing nevus patient is the concern for cosmesis and psychological problems as they cause facial disfigurement and are unacceptable for the patient. It often arises at the eyelid margin and may be flat, elevated, dome shaped and even pedunculated. They are well circumscribed, tan in color and often feature deep brown pigmentation. The larger form of nevus is reported to cause ptosis, however visual disturbances are a rare finding. In course of time, there is 2-30% risk of malignant change in the nevus giving rise to malignant melanoma. 4
If a small congenital nevus of eyelid is growing at the same rate as the child and is not changing in any other way, the usual practice is not to remove it until the child is old enough to co-operate with a local anesthetic injection, usually around the age of 10 to 12 years. Even then, removal is not essential. The aim of the treatment is to reliably remove the lesion with minimal functional impairment, to improve the cosmesis, and to prevent malignant transformation.
Reasons to consider surgical removal includes unsightly appearance, a recent change in the lesion (darkening, lumpiness, increasing size) and melanoma-like appearance (irregular shape, variegated color). There are several treatment options available for eyelid kissing nevus management which include cryotherapy, blepharoplasty, excision and skin grafting and CO2 laser. Reconstruction can be done by various methods including the entire reconstructive ladder with both one and two-staged approaches. Complications that may occur after reconstruction surgery includes graft or flap failure, infection, wound dehiscence, bleeding or hematoma and irritable or itchy scar. 5
The alternate treatment option remains radiofrequency ablation using micro-dissection technique. Radiofrequency ablation has been used in many minimal invasive procedures in the past like in heart arrhythmia, 6 venous malformation, 7 knee osteoarthritis 8 and periorbital syringoma. 9, 10 It has different effects under various temperature settings. It causes contacting tissue molecular oscillation by electromagnetic wave passing through the treatment electrode and good hemostatic effect on the ablated tissue. Radiofrequency ablation has multiple advantages over traditional operational methods with feasibility of accurate control, less collateral damage and limited complications. But till date, no study reported effectiveness of radiofrequency ablation in kissing nevus treatment.
Case Report
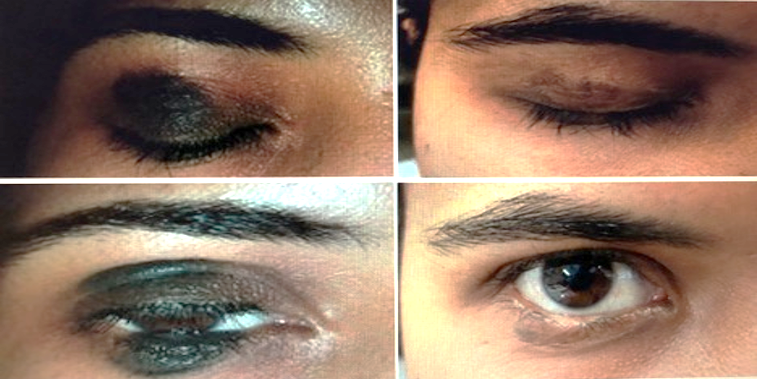
We report a case of 27 year old female who presented with history of having a painless, black colored, non-progressive swelling over right upper and lower eyelids since birth. She seeked medical advice only for cosmesis purpose. On examination, the nevus was non-tender, non-ulcerative, non-proliferative with verrucous edges and hypertrichosis, covering approximately 50% of both right upper and lower eyelid margins on right side. On eyelid closure, both nevi came in complete contact with each other, acquiring contiguity and appearing as a black circular spot on right eye and resembled a single entity (Figure 1). Conjunctiva, sclera and cornea were spared from pigmentation and rest ophthalmic examination was essentially normal.
Figure 1
Kissing nevus of the right eyelid and looking like as one whole nevus on attempted eyelid closure

Patient was planned for removal of right eye upper lid and lower lid divided nevus using micro-dissection radiofrequency ablation technique (MRA technique). Since the nevus was quite extensive, the entire procedure was completed in two sittings with an interval of 4weeks in between under local anesthesia. Patient was treated using the Radiofrequency surgery unit (Figure 2).
Principle of radiofrequency surgery unit
Radio Frequency surgery units operate at a high 4MHz – a factor of between 8 to 10 times higher than conventional low frequency electrosurgery diathermy units. Advanced Radio wave surgery works because living tissue exhibits a resistance to the close proximity of the 4 MHz of high frequency radio energy. This resistance will induce localized heat at temperatures high enough to vaporize the moisture content within the individual tissue cells, causing each cell to be destroyed, a process called volatilization. At 4MHz, thermal tissue alteration is limited to within 20 microns of the surgical site. That is a factor of 100 times less damaging than conventional electrosurgery. Clinically, the Radio Wave patient does not become part of an electrical circuit and the active electrode remains cold at all times. In high frequency Radiosurgery the antennae plate is simply attached to the patient’s calf or other muscle mass. It then picks up radio waves from the small active operating electrode completing a radio wave circuit. When this cutting electrode is in contact with the target issue, volatilization occurs and heat is only induced in that cell. Most importantly there is no peripheral charring or eschar and rapid healing is promoted.
Treatment protocol
The 5% iodophor conventionally disinfected the skin, and 2% lidocaine with adrenaline was used for local anesthesia. The treatment was performed under operating microscope under 10X magnification using the radiofrequency surgery device. During the process, surgeon could observe whether there was any residue, whether the radius of margin was smooth, and removing the lesion to the bottom to form a solidified protective layer. After the first sitting, the patient was informed of postoperative precautions, such as keeping the wound clean and waiting for natural healing after crust falling off. (Figure 3)
After 4 weeks, patient was taken up for 2nd sitting and ablation was stopped after all the visible pigment tissue was removed and normal tissue became visible, shaping the basilar part to get good cosmetic results, avoiding thermally damaging the lower dermis as far as possible to minimize the side effect. (Figure 5)
The procedure was successful with no scar or tissue loss or any palpebral margin deformation. (Figure 5) The patient was discharged with a healthy outcome and with no evidence of recurrence till date i.e almost after 18 months. Hence, radiofrequency ablation for kissing nevus showed significant efficiency and should be considered as an alternative and less invasive method than surgical excision.
Discussion
Nevus, a Latin word for “maternal impression” or “birth mark,” indicates a circumscribed, nonneoplastic skin or mucosal lesion which usually present at or soon after birth. Melanocytic nevus, a type of nonvascular epidermal nevus, is a benign proliferation of melanocytic cells, which are arranged in nests in epidermis, dermis, or other tissue. Congenital naevi occur in almost 1% of all newborns. Congenital divided nevus of the eyelids is a rare form, usually involving contiguous portions of the unilateral upper and lower eyelid margins. Patients are usually asymptomatic and seek medical attention for cosmesis; but a large nevus can cause mechanical ptosis which may lead to stimulation deprivation amblyopia.
Prophylactic surgical removal of a nevus
The following factors should be considered prior to prophylactic surgical removal of a nevus.
Prophylactic excision of a small lesion may be delayed until an age when the patient is old enough to make an informed choice.
Small or medium-sized congenital melanocytic naevi are at low risk for developing malignant change
Irregular, lumpy or thick lesions or lesions that are difficult to clinically assess may have a lower threshold for consideration of surgical excision, so as not to miss a melanoma.
50% of melanomas diagnosed in those with giant congenital melanocytic naevi occur at another body site such as within the central nervous system. Therefore, surgical excision of the lesion may not eliminate the risk of melanoma.
Large or giant melanocytic lesions may be too large to excise completely
Large lesions may require a skin flap or graft to close the surgical defect
If patient of kissing nevus has a history of growth, alteration in pigment pattern, vascularity, ulceration and associated inflammation, he should undergo excision biopsy as soon as possible because it carries a risk of 2-30% of malignant transformation into malignant melanoma.
Other treatment options for a congenital melanocytic nevus
Dermabrasion
Dermabrasion can allow partial removal of a large congenital nevus; deeper nevus cells may persist. Dermabrasion may lighten the color of the nevus but may not reduce hair growth within it. It can cause scarring.
Tangential (shave) excision
Tangential or shave excision uses a blade to remove the top layers of the skin (epidermis and upper dermis). This may reduce the pigmentation but the lesion may not be completely removed. Shave excision may result in significant scarring.
Chemical peels
Chemical peels using trichloroacetic acid or phenol may lighten the pigmentation of a superficial (surface) congenital nevus that is located in the upper layers of the skin. Techniques that result in partial removal of a congenital nevus can make the lesion more difficult to assess for malignant transformation during long term follow up. 8
Laser ablation
Laser treatment is considered one of the best alternative if surgical intervention is not possible. It may result in lightening of the lesion with minimal or no scarring. Suitable devices include:
Multiple stage mosaic punching excision of the congenital divided nevus using a 10,600-nm CO2 pulsed laser is a successful technique for removing congenital melanocytic nevus specially when lesion is treated early in life and nevus cells are still limited to the superficial dermis. If the nevus involves the deep dermis and subcutaneous tissue, then full thickness excision followed by full thickness skin grafting is preferred choice of treatment.
Radiofrequency ablation
MRA technique for removal of eyelid kissing nevus has not been reported before. Radiofrequency ablation microsurgery achieves the goal of precise and targeted eradication of lesions. It has multiple advantages, including short treating time, no bleeding during operation, mild collateral damage, forming protective layer on wound after treatment, rapid wound healing, no scar formation, disposable treatment electrode, no cross infection, which meet the need of clinical practice. The postoperative inflammatory reaction was light.11 At the same time, radiofrequency ablation avoids suture and its associated adverse post-operation complications.12
Therefore, radiofrequency ablation microsurgery can completely eradicate the eyelid nevus, and make patients achieve aesthetic appearance. Therefore, MRA technique is a highly accurate, practical and effective treatment in removing eyelid nevus, which possesses a potential of clinical recommendation. Further investigations regarding this innovative therapeutic approach is warranted.
Conclusion
Kissing naevi of eyelids are usually cosmetically unacceptable causing problems like depression and a feeling of low confidence. It can cause functional problems like ectropion of lower lid, ptosis and visual field defects. There are several treatment options available including CO2 laser ablation, cryotherapy, blepharoplasty, excision and skin grafting. With the advantage of simplicity, precision and effectiveness, radiofrequency ablation using micro-dissection technique can be recommended to treat kissing nevus with good cosmetic results and skin grafting with its associated drawbacks can be avoided.