- Visibility 154 Views
- Downloads 39 Downloads
- DOI 10.18231/j.ijooo.2021.073
-
CrossMark
- Citation
Post enucleation reconstruction of orbit using silicone orbital implant and dermis fat graft
- Author Details:
-
Mohammed Ather *
-
Rahmatunissa
-
S Saudhamini
-
T Shreya
-
Samra Wahaj Fatima
Introduction
If no orbital implant is placed, or if the implant is of insufficient size, the ocular prosthesis will have to be made larger than is desirable in an attempt to reduce the volume deficit, which manifests itself by an enophthalmic appearance and an upper eyelid sulcus deformity. The lower lid eventually becomes stretched, the ocular prosthesis becomes inferiorly and posteriorly displaced, the levator palpebrae superioris muscle loses its fulcrum of action, and the upper eyelid sulcus deformity becomes more exaggerated. The patient then exhibits features referred to as the post-enucleation socket syndrome (PESS).[1], [2]
PESS features are enophthalmos, An upper eyelid sulcus deformity, Ptosis or eyelid retraction, Laxity of the lower eyelid, A backward tilt of the ocular prosthesis.
The volume of an adult globe is approximately 8cc.[3] Besides the 8 cc. volume loss through enucleation, there can be additional soft tissue loss of 4cc, resulting in a total decreased volume of 12 cc.[4] The volume replaced by a 20 mm spherical implant is only 4cc.[5] A prosthesis may give an additional 1.5 to 4cc, therefore providing a total 5.5 to 8 cc of orbital volume replacement.[6] But still there will be deficit of 4 to 6.5cc of volume.[7]
Anophthalmic superior sulcus deformity can be addressed by a variety of techniques, including intra conal implants, sub periosteal implants or through direct augmentation of the superior sulcus.[8] Direct augmentation of superior sulcus using free fat or dermis-fat graft, temporo-parietal fascia has been described for many years. However when using graft materials, resorption may happen with time and temporo-parietal fascia flap surgery involve more complex surgery.
Purpose of this study is to perform enucleation, followed by silicon orbital implant and placing Dermis fat graft over it in single sitting and to study the results by measuring palpebral aperture height, enophthalmos, superior sulcus deformity and cosmesis after 3 months.
Materials and Methods
This is a prospective interventional study conducted at the Department of Oculoplasty and Orbital diseases of a tertiary care eye hospital between 2014-2016. 30 patients of which 16 were males and 14 were females were included in the study. Patients who underwent enucleation for painful blind eyes, Pthisical eyes and anterior staphylomas were included in the study. Patient who underwent enucleation for malignant conditions like Retinoblastoma and Malignant Melanoma were excluded from the study. Informed consent was obtained from adult patient and consent of one of the parent was obtained when the patient was under 18 years of age after explaining the procedure to them in their own language. All patients were examined by an experienced Ophthalmologist using Slit lamp, Snellens chart, Direct and indirect Ophthalmoscope, Exophthalmometer, Transparent scale.
Surgical profile investigations were done on all patients like, CBP, Hb estimation, complete urine exam, HIV, HBSAg. B Scan was performed on all eyes to be enucleated to rule out any intra ocular tumour. A Scan biometry of normal eye was done to determine axial length of eyeball. 2mm was substracted from axial length to determine the size of the Silicon spherical orbital implant to be implanted. [5], [6], [7]
After Pre anaesthetic check up adults were posted for enucleation under Four quadrant Block and Analgesia. All children were posted under general anaesthesia. First Dermis fat graft was harvested from upper and outer quadrant of buttock. Then enucleation was completed following standard steps. Four Recti muscles were held long. Then Silicon spherical orbital implant was placed in the posterior sub tenon’ space and Tenon’s capsule was sutured using 6’0 Vicryl sutures. Dermis fat graft which was harvested was trimmed according to the space available and placed over the Obital implant infront of Posterior Sub tenon’s capsule. Recti muscles were anchored to the edge of Dermis fat graft above, below, laterally and medially.
Conjunctiva was sutured to the edge of Dermis fat graft by interrupted 6’0 Vicryl sutures. Conformer was placed and Suture tarsorrhaphy was done. All patients were given Tablet. Ciprofloxacin 500 mg. BD for five days along with Analgesic Tablets. Topical Antibiotic eye drops were prescribed to be instilled at medial canthus.
All patients were examined on first Post operative day and discharged from hospital. They were called after 2 weeks for removal of Suture Tarsorrhaphy. They were instructed not to remove conformer and use topical antibiotic drops. They were called after 2 weeks to follow the conjunctivilisation of dermis. After 3 months conformer was removed and Prosthetic eye was implanted. Then Palpebral aperture height was measured using a transparent scale. Amount of Enophthalmos was calculated by exophthalmometer by taking the difference between the two eyes. Superior orbital sulcus fullness was documented by clinical photograph. If there was Superior orbital sulcus deformity present, it was measured by transparent scale. Cosmesis was judged by another doctor and attender of the patients.
Results
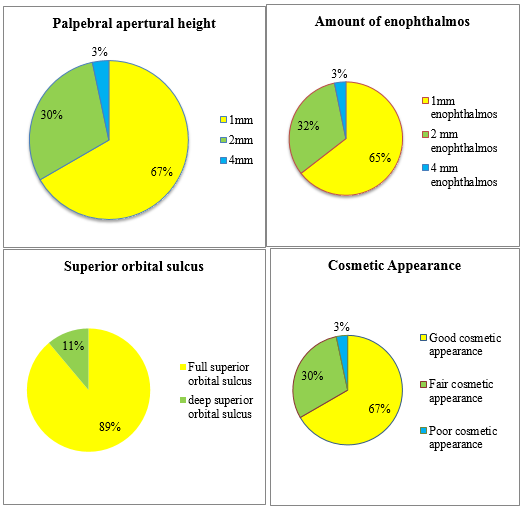
20 cases had 1mm difference in palpebral aperture height when compare to normal eye. 9 cases had 2mm, and one case had 4mm difference in palpebral aperture height.
enophthalmos with prosthesis was measured by taking the difference of exophthalmometer readings of two eyes. 20 cases had 1mm of Enophthalmos when compared to normal eye. 9 cases had 2 mm of enophthalmos, 1 case had 4mm of enophthalmos.
20 cases had fullness of superior orbital sulcus. 10 cases had 1-3 mm of superior orbital sulcus deformity.
Cosmetic appearance was judged by doctors and attenders of patient. 20 cases had good cosmetic appearance. Whereas 9 had fair cosmetic appearance, 1 had poor cosmetic appearance. The patient having poor appearance had bony contraction of orbit because of pthisical eye.








Discussion
Nunery, William R, Heinz, Grant W, Bonnin, et al. [9] In June 1993 have reviewed retrospectively enucleations and secondary anophthalmic socket sphere implantations for a 3 year period. They found the incidence of hydroxyapatite exposure following enucleation was 3 out of 27(11%).
The incidence of silicone sphere exposure following enucleation was 0 of 48(0%) and following secondary implantation was 1 of 30(3.3%).
So they believed that the hydroxyapatite anophthalmic sphere is associated with a higher incidence of exposure and postoperative inflammation when compared to silicone anophthalmic spheres
In the present study, the orbital implant was closed with tenons and dermis fat graft anteriorly. By this the implant exposure can be reduced because it is covered not only by tenons but also dermis fat graft which gives implant a good barrier to prevent exposure.
Kim NJ,, Choung HK, Khwarg SI, et al [10] have studied to determine if porous polyethylene orbital implant (Medpor) exposure can be prevented in retinoblastoma patients when the implant is placed in combination with a free orbital fat graft over the anterior surface. Implant exposure occured in 13 of 39 eyes (33.3%) that had conventional enucleation and medpor implantation, exposure did not develop in any of the 38 eyes that had the combined procedure with a free orbital graft. So they concluded that a free orbital fat graft is a simple, effective way to prevent orbital implant exposure in patients with retinoblastoma requiring enucleation
In the present study all three procedures i.e, enucleation, orbital implant and dermis fat graft were done simultaneously. This reduced the chances of implant exposure and the need for second surgery.
Lee BJ, Lewis CD, et al [11] in 2010 have tried to describe a technique for simultaneous secondary orbital implantation and dermis fat graft placement for exposed porous implants with significant conjuctival insufficiency. 4 patients underwent simultaneous dermis fat graft placement and secondary implantation for exposed and completely avascular orbital implants. The rectus muscles were advanced over the new implant to act as as the host bed for dermis fat graft. All patients tolerated a new prosthesis well, with adequate motility and cosmesis.
They concluded that simultaneous secondary implantation and dermis fat graft placement may adequately address avascular porous implant exposure with significant conjunctival insufficiency.
Jae Yeong Park and Hee Young Choi et al [12] from Korea in February 2015, investigated the clinical results of patients who have undergone simultaneous dermis fat graft and insertion of orbital implants in patients who are unable to put on an ocular prosthesis due to severe conjunctival sac contracture or large orbital implant exposure. Eight eyes were enrolled in the study and among them five eyes (62.5%) were diagnosed with orbital implant exposure and underwent orbital implant exchange and dermis fat graft, two eyes(25%) were anophthamic patients and underwent secondary orbital implant insertion and dermis fat graft. One patient (12.5%) underwent orbital implant insertion and dermis fat graft simultaneously during the evisceration operation. They followed up for 46.3 months and found for seven out of eight eyes, the results of wound healing process was successful. One patient underwent removal and reinsertion of the orbital implant with dermis fat graft and the wound in it healed well. After 5 months dermis fat re-graft was performed for orbital implant re-exposure and it was not exposed thereafter. Overall cosmetic appearance was satisfactory in each patient and all patients were able to comfortably retain a prosthesis. Hence they found that undergoing dermis fat graft simultaneously when performing orbital implant insertion is effective for replacement of the conjunctival sac and orbital volume.
In the present study also we observed that after placing a dermis fat graft over the orbital implant, there is good replacement of orbital volume and fullness of superior orbital sulcus and sufficient lower conjunctival fornix formation to comfortably accommodate prosthesis.
Conclusion
Post enucleation socket syndrome (PESS) manifests by an enophthalmic appearance and an upper eyelid sulcus deformity. These features can be minimised by using an orbital implant and dermis fat graft over it as primary procedure. Dermis fat graft when used simultaneously with the orbital implant soon after enucleation can prevent complicated secondary surgery ie implant exchange and then dermis fat graft over it after implant exposure has occurred.
Thus the placement of the orbital implant and dermis fat graft soon after enucleation resulted in good cosmetic appearance in most of the patients. There was less difference in palpebral aperture height, less amount of enophthalmos, and fullness of superior orbital sulcus, in comparison with the normal eye.
Dermis fat graft was used previously only after there is extrusion of the implant. So rather than waiting for the extrusion or exposure of implant to occur and then taking up for secondary surgery. Its better to prevent exposure by using the implant and dermis fat graft at same time after enucleation. Thus, we have combined two different procedures in one sitting and have seen good cosmetic results, improved patient compliance, prevention of implant extrusion , exposure and comfortable retention of ocular prosthesis.
By using a dermis fat graft over an orbital implant, the superior orbital sulcus deformity can be prevented because there is good augmentation of orbital volume
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- F J Steinkogler. The treatment of the post-nucleation socket syndrome. J Craniomaxillofac Surg 1987. [Google Scholar] [Crossref]
- C Byeung-Hun, L Sang-Hyeok, C Wha-Sun. Correction of Superior orbital sulcus deformity. Korean J Ophthalmol 2005. [Google Scholar]
- J A Nerad, K D Carter, M A Alford. Disorders of the orbit: anophthalmic Socket: Oculoplastic & Reconstructive Surgery. 2008. [Google Scholar]
- B Leatherbarrow. Oculoplastic Surgery Brian Leather Barrow. 2nd Edn.. 2011. [Google Scholar]
- S Shah, Y Shah. AIOS CME Series No. 15 Implants in Ophthalmology . . [Google Scholar]
- S A Kaltreider. The ideal ocular prosthesis: analysis of prosthetic volume. Ophthal Plast Reconstr Surg 2000. [Google Scholar]
- P L Custer, K M Trinkaus. Volumetric determination of enucleation implant size. AJO 1999. [Google Scholar]
- C T Shaw, M O Hughes, M Kirzhner. nophthalmic syndrome: a review of management. Ophthalmo Plasty Reconstructive Surg 2014. [Google Scholar]
- W R Nunery, G W Heinz, J M Bonnin, R T Martin, M A Cepela. Exposure rate of hydroxyapatite spheres in the anophthalmic socket: correlation and comparison with silicone sphere implants. Ophthal Plast Reconstr Surg 1993. [Google Scholar] [Crossref]
- N J Kim, H K Choung, S I Khwarg, Y S Yu. Free orbital fat graft to prevent porous polyethylene orbital implant exposure in patients with retinoblastoma. Ophthal Plast Reconstr Surg 2005. [Google Scholar]
- B J Lee, C D Lewis, J D Perry. Exposed porous orbital implants treated with simultaneous secondary implant and dermis fat graft. Ophthal Plast Reconstr Surg 2010. [Google Scholar]
- J Y Park, H Y Choi. Clinical Outcomes Following Simultaneous Orbital Implant Insertion Operation and Dermo-Fat Graft for Anophthalmos Patients. J Korean Ophthalmol Soc 2015. [Google Scholar]
How to Cite This Article
Vancouver
Ather M, Rahmatunissa , Saudhamini S, Shreya T, Fatima SW. Post enucleation reconstruction of orbit using silicone orbital implant and dermis fat graft [Internet]. IP Int J Ocul Oncol Oculoplasty. 2021 [cited 2025 Sep 13];7(4):348-353. Available from: https://doi.org/10.18231/j.ijooo.2021.073
APA
Ather, M., Rahmatunissa, , Saudhamini, S., Shreya, T., Fatima, S. W. (2021). Post enucleation reconstruction of orbit using silicone orbital implant and dermis fat graft. IP Int J Ocul Oncol Oculoplasty, 7(4), 348-353. https://doi.org/10.18231/j.ijooo.2021.073
MLA
Ather, Mohammed, Rahmatunissa, , Saudhamini, S, Shreya, T, Fatima, Samra Wahaj. "Post enucleation reconstruction of orbit using silicone orbital implant and dermis fat graft." IP Int J Ocul Oncol Oculoplasty, vol. 7, no. 4, 2021, pp. 348-353. https://doi.org/10.18231/j.ijooo.2021.073
Chicago
Ather, M., Rahmatunissa, , Saudhamini, S., Shreya, T., Fatima, S. W.. "Post enucleation reconstruction of orbit using silicone orbital implant and dermis fat graft." IP Int J Ocul Oncol Oculoplasty 7, no. 4 (2021): 348-353. https://doi.org/10.18231/j.ijooo.2021.073
