Introduction
Rhinosporidiosis is a parasitic disease and presented as a chronic localized granulomatous disease caused by Rhinosporidium seeberi.1 Rhinosporidiosis is a common disease and endemic in India as well as Sri Lanka but quite is sporadic in other parts of the world. 2, 3 Most common site of involvement is nasal mucosa, followed by ocular involvement. Other natural orifices such as the penis, urethra, anus, vagina, skin 4 may also be involved; few cases of disseminated rhinosporidiosis have also been reported in the literature.5, 6 Rhinosporidiosis of the eye and adnexa is termed as oculosporidiosis. 7 Clinically, oculosporidiosis appears as a friable polypoid mass, causing a foreign body sensation, irritation and watering from the eye, and no effects on vision according to fewer case reports. 8 Oculosporidiosis commonly occurs in young and younger adults (15–40 years) with a predominance in males. 9
Here, we present an interesting case of oculosporidiosis. How the patient was diagnosed and treated is also provided, along with the recent literature review.
Case Report
A 25-year-old male patient was presented with a swelling over the right lower periorbital area for the last 3 years. On examination, the swelling was pinkish in color with an oblique linear scar over it due to previous surgical intervention [Figure 1]. On palpation, the swelling was soft, nontender, and fixed with the deeper tissue.
Figure 1
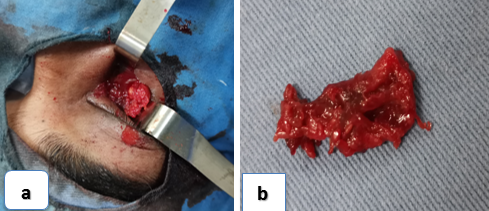
a: The patient presented right orbital swelling with a scar on it after two months of primary treatment.
b: The patient was initially introduced on the right lower orbital lesion diagnosed as orbital abscess and drained the abscess locally two months ago.

Two months ago, he was treated as a case of orbital abscess of his right eye for which FNAC was done, then incision and drainage were made by an ophthalmologist in his local area; it took around 2 weeks for the wound to heal. Although there was an initial reduction of the size of the swelling for a month, the swelling started to grow again for the last one month.
He was treated at the tertiary-based eye hospital, Dhaka. CT Scan of orbit was done and nasal swabs were collected. Contrast-enhanced computed tomography scan of the orbit showed soft tissue lesion (3.2 x2.3x1.6 mm) with intralesional loculated fluid collection in the inferomedial aspect of the right orbit. Mild heterogeneous enhancement of the lesion compresses the right eyeball [Figure 2 a,b]. The impression of the radiologist was an inflammatory lesion of the lacrimal sac with pyocele and bilateral maxillary sinusitis.
Figure 2
a,b: CT scan of orbit showing soft tissue mass in the lacrimal sac fossa with a bony breach and extension into inferomedial aspect of orbit; c: Repeat CT scan of orbit showing enhancing soft tissue mass in the floor of the right orbit.

Repeat incision and drainage were conducted by an ophthalmologist at that hospital. After external healing of the wound, the swelling started to grow again for the last one month. After that, he came to us (Dept. of ophthalmology, BIRDEM General Hospital) for treatment.
On examination, his visual acuity was found to be normal; conjunctiva was normal; syringing through both puncta of his right upper and lower eyelid proved the patency of the lacrimal drainage system. Repeat CT scan of orbit was done which showed enhancing two soft tissue masses in the floor of the right orbit measuring about (1.7x1.4) and (3.2x1.2) cm with thickening of perilesional fat. [Figure 2c]
His routine blood investigation along with erythrocyte sedimentation rate was normal. The patient was tested negative for the COVID-19 test. His X-ray chest was done for a routine pre-anesthesia check-up, which was found to be normal.
Hence, with a preoperative diagnosis of orbital swelling due to lacrimal sac pyocele, we decided to explore the area surgically. The operation was performed under general anesthesia. An incision was placed over the old scar extending medially up to the medial canthal ligament. On exploration, we found an ill-defined soft tissue mass adherent with the surrounding soft tissues; meticulous dissection was done and the swelling was found to be extending deep into the orbit. As the lacrimal sac was closely adherent with the mass, it was removed. [Figure 3a,b]. Extra-ocular muscles were not involved and intraoperative tests were done to check their functions. An Electro-cauterization of the wall of the cavity was done to achieve hemostasis; the wound was then closed.
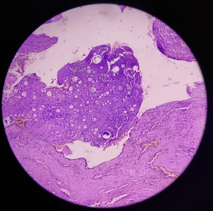
Histopathological examination of the specimen was conducted. Sections from the orbital cyst and lacrimal sac showed tissue-lined partially by stratified squamous epithelium and partially by columnar epithelium. Sub-epithelium showed sporangia with endospores. Surrounding tissues showed chronic inflammatory cell infiltrate [Figure 4]. Thus, a diagnosis of orbital rhinosporidiosis was made.
The patient had early recovery and was discharged on the 3rd postoperative day with oral antimicrobial therapy (dapsone 100 mg/day, for 6 days a week, for 6 months). Before discharge, a thorough ENT cheek-up was done with a nasal endoscope and fiberoptic laryngoscope to look for any such lesion in the upper respiratory passage, but no such lesion indicating infestation by Rhinosporidium in that area was found. There was no sign of recurrence in the last 6 months follow-up. [Figure 5]
Discussion
Oculosporidiosis is usually found among 10-15% of rhinosporidiosis cases. In the cases of oculosporidiosis, the commonest affected tissue is conjunctiva (77.6%), followed by lacrimal sac (26%) with or without conjunctiva involvement. Kuriakose ET described the clinical features of the lacrimal sac oculosporidiosis, as it may present with a painless, soft, swelling in the lower eyelid; which is fluctuating to the touch; there may be a history of bleeding from the nose, and haemolacria is seldom completely obstructed. 8
In our case, though there was no bleeding from the nose, other features were present. But still, we missed the diagnosis because isolated oculosporidiosis of the lacrimal sac is very rare. So it becomes challenging to suspect a secluded lacrimal sac is swelling to be due to infestation by Rhinosporidium. 10 They described a patient with recurrent painful swelling of the right lower eyelid, who was diagnosed elsewhere as a case of chronic dacryocystitis. They diagnosed it as a case of idiopathic orbital inflammatory disease.11 Final diagnosis was made only after a tissue biopsy from the lacrimal sac area.
A CT scan of the orbit may reveal an enlarged lacrimal sac, along with polypus mass inside the sinuses, thus helping to diagnose the lesions of rhinosporidiosis. However, in this case, the CT scan of the orbit showed enhanced heterogenous lesion involving the right lacrimal sac that showed a lacrimal abscess, paranasal sinuses were revealed as normal study. Thus, he was diagnosed with a chance of lacrimal sac pyocele. However, in suspected cases, the histopathological examination can confirm this disease, which shows characteristic features as numerous sporocysts in various stages of maturation.
Complete surgical excision is the mainstay of the Management of lacrimal oculosporidiosis; 5 but there is a very high chance of recurrence, as reported by two large case series. 7 The recurrence may occur due to incomplete removal of the infested sac. 10, 11, 12
It is often difficult to dissect the involved lacrimal sac becomes because of the risk of severe intraoperative bleeding. 13 In our case, we experienced the same, and the bleeding was controlled by gel foam application. After excision of the lesion, copious irrigation with 5% povidone-iodine solution and 5 mg/ml amphotericin-B have also been tried with good results. 12
Adjuvant antimicrobial dapsone therapy is used as an additional measure to reduce the possibility of recurrence as it has been found to halt the maturation of spores and promote fibrosis in the stroma.12, 14 Although, some study suggests that dapsone therapy may not be very effective. 15
In association with surgery, dapsone may be used to prevent the maturation of sporangia and promote fibrosis. 16 Histopathological analysis revealed the confirmed diagnosis, with a demonstration of a fibrous stroma with several thick-walled sporangia at different stages of maturation and containing numerous endospores. 17, 18
Conclusion
Isolated oculosporidiosis involving the lacrimal sac and presenting as a periorbital swelling is a rare clinical finding that can initially be misdiagnosed. In this case, it was wrongly diagnosed as a pyocele. The lesion, in such cases, must be surgically excised. Surgical excision followed by histopathological examination is vital for any suspicious lacrimal sac lesion. Postoperatively, dapsone therapy may be an additional measure to reduce the possibility of recurrence.