Introduction
The term “functional block” was originally used by Demorest and Milder in 1955 to encompass the concept of lacrimal drainage dysfunction in the presence of anatomical patency in the era when lacrimal imaging was practically non-existent.1 The addition of ‘positive Jones I with negative Jones II tests and normal dacryocystograms’ elaborated this definition further. Alternate nomenclatures include physiological dysfunction, functional disorders, partial functional disorders, functional nasolacrimal blockage, functional acquired epiphora.
At present dacryocystorhinostomy (DCR) is the treatment of choice in patient of functional epiphora. The outcome of DCR surgery in these challenging patient is less clear with reported success rate ranging from 50-94%.2, 3, 4, 5 DCR surgery is a procedure that aims to eliminate fluid and mucus retention within the lacrimal sac and to increase tear drainage for relief of epiphora.
As surgery may not be the best option in all patients especially in the elderly population. Now injection Botulinum toxin has been introduced as an alternative management to surgical approach.
Botulinum is a neurotoxin which reversibly blocks acetyl-choline release in cholinergic nerve terminals of the neuromuscular synapse and of autonomic nerve fibers. Injection of Botulinum toxin A in the lacrimal gland blocks the presynaptic release of acetylcholine which is required for tear secretion,6 Therefore injection of botulinum toxin in lacrimal gland can be an alternative treatment in functional epiphora, canalicular obstruction, gustatory hyperlacrimation and gustatory sweating(Frey’s syndrome). Botulinum injection in the lacrimal gland is devoid of the risks and complications of an invasive surgery and local or general anesthesia. Injection can be performed in an outpatient clinic. This technique is easy, minimally invasive, and less time consuming, compared with surgery. However, its effect is dry eye, transient ptosis and diplopia.7, 8, 9
There are fewer studies and literatures which have addressed about the outcome of DCR and Injection Botulinum toxin in the management of functional epiphora. And all the previous studies have only reported about the outcome of single intervention either DCR or Injection Botulinum toxin. Different studies done worldwide show different results regarding the success rates of the two procedures. And there is no study evaluating the outcome of this treatment. So we compared the outcome of DCR and Inj Botulinum in patients with functional epiphora.
Materials and Methods
This was a hospital based prospective, comparative, interventional study from August 2018 to July 2019 with follow up period of 6 months upto January 2020 conducted at Tilganga institute of ophthalmology. A total of 45 patients diagnosed as functional epiphora and meeting all inclusion criteria were enrolled in this study. Patient were included if they: had epiphora with patent nasolacrimal irrigation, had retention of dye during fluorescein dye disappearance test (FDDT) and age above 18years. Exclusion criteria included patients with ocular irritant disease, dry eye syndrome, eyelid malposition, patient with history of previous trauma and surgery to lacrimal region or who had granulomatous or inflammatory diseases, patient with history of using anti-glaucoma medication like pilocarpine and ecothiophate or under radioactive iodine therapy, chemotherapy or radiotherapy, facial nerve palsy. Informed consent was taken from all the persons enrolled. The study was approved by institutional review board of National Academy of Medical Sciences.
Out of total 45 patients, 20 patients underwent external dacryocystorhinostomy (DCR) and 25 patient received injection botulinum toxin as per their will. patients with the history of epiphora were asked for detail history. All patients underwent ophthalmic examination which included visual acuity, external examination, slit lamp examination, FDDT and lacrimal syringing. Epiphora was graded according to Munk score preoperatively.
The external DCR was done under local anesthesia.4% lidocaine was instilled into conjunctival sac, 2-3 times before preparation. Patient on supine position, aseptic cleaning and draping of operating eye was done. Dorsonasalis, infraorbital and infratrochlear nerve block was done at incision site using 2% lidocaine with adrenaline 1:100,000 and 0.5% bupivacaine. Nasal packing was done with 4% lidocaine with adrenaline 1:100,000 and oxymetazoline 0.05%.A vertical incision was given parallel to nasal bridge just medial to the site of angular vessels (10mm from medial canthus) with a 15 no. Bard-parker blade. Orbicularis muscle was dissected, periosteum was separated from bone medially and laterally to the anterior lacrimal crest with the periosteum elevator. The suture running between the frontal process of the maxilla and the lacrimal bone was infractured using the periosteum elevator and a wide bony defect was created using Kerrison bone punch. H shaped incision given at postero-inferior part of lacrimal sac with long anterior flap and short posterior flap. Similarly corresponding incision was given at nasal mucosa with short posterior flap and long anterior flap. Then posterior flap of both lacrimal and nasal mucosa was excised. Finally the anterior flap of lacrimal sac and nasal mucosa was sutured with 6-0vicryl in interrupted fashion. Orbicularis was closed with vicryl 6-0 in interrupted fashion. Nasal packing was done with 4% lidocaine with adrenaline and oxymetazoline. Wound was covered with sterile gauze. Oral antibiotics, analgesic were given to the patient on same day of operation. And patient was advised to elevate head while sleeping, avoid nose blowing, hard food.
Botulinum injection was given as follows: first the topical drop of 4% Lidocaine was instilled 2-3 times before injecting Botulinum toxin in the affected eye. Botulinum toxin was diluted with 1ml of sterile preservative free saline (50units/1ml).5 units of Botulinum toxin was withdrawn in 1ml syringe with the 23gauze needle then replaced with 26 gauze needle, Patient was advised to look down and medially and the upper lid was retracted laterally so that the prolapsed palpebral portion of lacrimal gland was visible. Then Botulinum toxin A was injected into palpebral lobe of the lacrimal gland. Patient were prescribed topical lubricants after the procedure.
A follow-up examinations of patients was done on 1st post-operative day (POD),7th day,1 month,3 month,6 months after surgery and post-injection. In each follow-up the patients who had undergone DCR surgery were examined for post operative complication including periocular hematoma, bleeding, cheese wiring of puncta and wound infection. Eye drops of combined topical antibiotics and steroid were given 6hourly for 1 week and Tablet Amoxicillin 500mg +Clavulinic acid 125mg three times a day for 1 week, Tablet Paracetamol 500mg three times a day for 3days, Tablet Trypsin and chymotrypsin 100000 AU three times a day for 5days were continued. Suture removal was done 1 week after surgery. Silicone tube was removed after 6 weeks. Munk score was asked in each follow-up.Surgical success was defined as symptomatic reduction in epiphora or Munk score of 0 or 1 at the end of 6 months after surgery. Dye disappearance test was done in each follow up and wound scar was noted.
Incase of injection botulinum toxin patient were followed up same as in DCR surgery. In each follow-up they were asked for any complications like ptosis, diplopia, dry eye. Similarly Munk score was asked in each follow-up and schimer’s test was done to rule out dryness of eye.
In each follow up symptomatic improvement was graded with Munk score postoperatively along with fluorescein dye disappearance test. The success was defined by symptomatic improvement of epiphora which was graded by Munk score at each follow-up. Munk score of 0 and 1 was considered as successful. Intraoperative and postoperative complications were also evaluated. All the DCR and injection Botulinum toxin were performed by the experienced oculoplastics surgeons at our hospital.
Table 1
Epiphora grading according to Munk 7
Results
In our study total of 45 patient were enrolled. If the fellow eye of enrolled patient was also affected then it was also intervened and was also included in the study. Out of 45 patients, 20 patients underwent DCR surgery and 25 patients received injection Botulinum toxin. Mean age in external DCR group was 49.55 years and in injection Botulinum group was 48.12 years. Out of 45 patients, 32(71.11%) patients were female and 13(28.89%) patients were male, in the ratio of 2.4:1.17(37.78%) patients had right eye involvement, 19(42.22%) patients had left eye involvement and 9(20%) patients had both eye involvement.
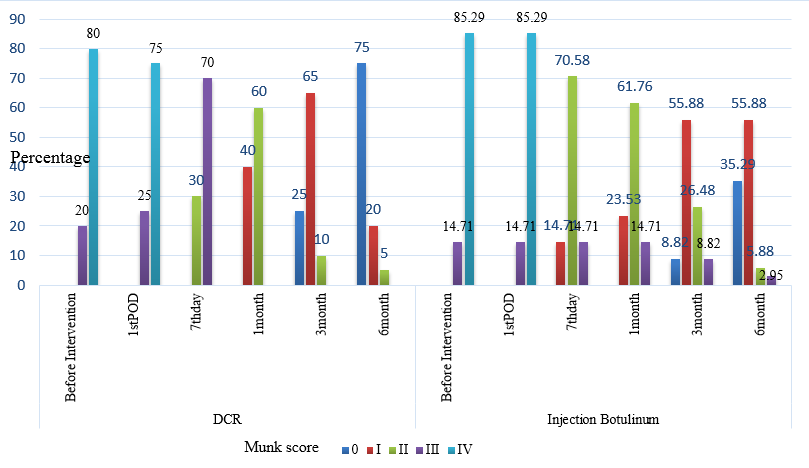
In this study 20 eyes in external DCR group, the mean Munk score was 3.8 before intervention and at the 6 month follow-up mean Munk score was 0.35. Out of 34 eyes in injection Botulinum group mean Munk score was 3.85 before intervention where as mean Munk score in this group was 0.78 at the 6 month follow-up. The Munk score before and after intervention was statistically significant (p<0.05), which shows there was improvement in epiphora in both groups. P-value was calculated using Wilcoxon signed rank test.
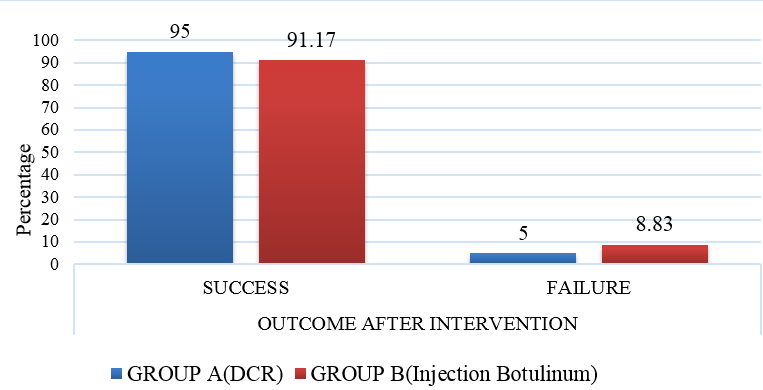
During fluorescein dye disappearance test, there was retention of the dye present in all i.e 54(100%) eyes before intervention where as at 6 month follow-up 19(95%) eyes in External DCR group showed no retention, 1(8.83%) eye had retention and 31(91.17%) eyes had no retention of dye in injection Botulinum group and 3(8.82%) had retention of dye.
The overall success rate at 6 months after surgery for External DCR is 95% and that of Injection Botulinum toxin is 91.17%.Out of 34 eyes, there was no symptomatic improvement i.e still watering in 1(5%) eye who underwent external DCR and 3(8.82%) eyes who received Injection Botulinum toxin. The overall success rate in both the group was not statistically significant, p>0.05. Fisher-Exact test was used to calculate P-value.
Among 20eyes, in external DCR group 1(5%) had bleeding as post-operative complication where as out of 34 eyes in injection Botulinum toxin group 10(29.41%) eyes had dry eye at the end of the 6 months follow-up. Among 10 eyes who developed dry eye, 1(2.94%)eye also had diplopia, 1 (2.94%)eye had subconjunctival hemorrhage and 2(5.88%)eyes had ptosis as early complications. Diplopia lasted for 3 weeks and ptosis resolved by 4 weeks of duration. Post-interventional complications between two groups was statistically significant (p-value <0.05). Fisher-Exact test was used to calculate p-value.
Table 2
Laterality distribution in both group
|
Eye |
External DCR (No .of patient) |
Injection Botulinum (No.of patient) |
|
Right eye |
10 |
7 |
|
Left eye |
10 |
9 |
|
Both eye |
|
9 |
|
Total |
20 |
25 |
Table 3
Types of Post-interventional complications
Discussion
The term ‘functional nasolacrimal duct obstruction’ has been used to describe patients with epiphora with evidence of abnormal tear drainage, but where the nasolacrimal duct is partially or completely patent on syringing.10 Epiphora in the presence of a patent lacrimal drainage system (LDS) confirmed either clinically or radiologically is a difficult condition to address. Based on the existing literature, consensus is still lacking regarding what truly constitutes functional epiphora. The most preferred tests according to Conway’s survey are nasolacrimal irrigation, primary and secondary dye test (Jones I and Jones II) and fluorescein dye disappearance test(FDDT).11 Imaging with dacryocystography or dacryoscintigraphy may provide further information for diagnosis and management. The treatment options are controversial and vary from simple eyelid tightening to lacrimal intubation and even dacryocystorhinostomy (DCR), with reported success rates ranging from 50 to 90%.2
Botulinum toxin A had established role in the treatment of ocular motility disorders, therapeutic ptosis, spasmodic torticollis, essential blepharospasm/hemifacial spasm and facial wrinkles. However its use in hyperlacrimation has been limited to that associated with aberrant regeneration of autonomic nerve fibers following facial nerve palsy. In these few cases it has been shown to give a marked and prolonged reduction in epiphora symptom. Botulinum toxin A injected into the lacrimal gland to reduce tear production is a new approach to the management of functional epiphora.7
Our comparative study showed that most of patient in external DCR group was in >60(30%) years and in injection Botulinum group were in 18-30(24%) years, 51-60(24%) years and >60 (24%) years. This indicates that functional epiphora is more common in elderly age group. Abnormal lacrimal drainage may be an exaggeration of the aging process which is associated with slowing of nasolacrimal transit time.12 The effect of lacrimal pump is reduced with increasing age probably as a result of decreasing orbicularis muscle tone, increasing fibrosis in the nasolacrimal drainage system and alteration in medial canthal tendon anatomy. 12, 13 The mean age of presentation in this study was 49.55 years (age range 18-73) in external DCR group which was similar to Simsek et al1 study which reported mean age of patients who underwent external DCR for the treatment of functional nasolacrimal duct obstruction as 48.68 years and in our study the mean age for injection Botulinum group was 48.12 years(age range 18-82) which was less than a study by Whittaker et al7 which reported mean age of patient who underwent injection Botulinum as 60 years(range 41-84years) in their study. The difference in mean age of two study may be because of the wide age range i.e from 18yrs to 82yrs of patient enrolled in Botulinum toxin group in our study. The mean age distribution between the external DCR and injection Botulinum group was statistically not significant in our study, p-value >0.05.
In this study out of 45 patients, 32(71.11%) were female and 13(28.89%) were male and ratio was 2.4:1. O’Donnel et al14 reported female predominance 39(76.47%) and male 12(23.52%) with ratio of 3.2:1 which was similar to our study. Brewis et al15 study constituted 63% female and 37% male patient who underwent dacryocystorhinostomy for functional lacrimal obstruction. In a study performed by Delaney et al16 reported 73.46% female and 26.54% male patients who underwent external DCR for acquired partial nasolacrimal duct obstruction. Singh et al2 have reviewed several articles published in English till 2018 on functional epiphora and found different rate of prevalence of functional epiphora in different studies however female prevalence was more than male in most of those studies.
In this study out of 45 patients, 17(37.78%) patients have right eye involvement, 19(42.22%) have left eye and 9(20%) have both eye involvement. Brewis et al15 study showed results involving right eye in 31(46%) cases and left eye in 37(54%) cases. Peter et al17 reported out of 42 patients who underwent external DCR for patent but non-functioning lacrimal system, 4(9.52%) patients had bilateral eye involvement and 38(90.47%) had unilateral involvement. In our study among 20 patients who opted for external DCR, 10(50%) had right eye involved and 10(50%) had left eye involved. Among 25 patients who opted for injection Botulinum, 7(28%) had right eye involved, 9(36%) had left eye involved and 9(36%) had both eye involved. So the reason behind patients opting for injection botulinum toxin over external DCR in case of both eye affected may be the less invasive, easy, less destructive and less painful procedure.
In this study, watering is the most common symptoms present in 20(100%) eyes in external DCR group and 34(100%) eyes in injection Botulinum group along with associated symptoms like intermittent discharge 6(30%) eyes in external DCR group, 4(11.76%) eyes in injection Botulinum group and foreign body sensation 8(40%) eyes in external DCR group and 6(17.64%)eyes in injection Botulinum group. As far as symptoms are concerned a similar level of frequency and severity of epiphora has been reported among the patients with primary acquired nasolacrimal duct obstruction(PANDO) and patients with functional nasolacrimal duct obstruction(FNLDO) inspite PANDO being complete anatomical obstruction of tear drainage. Comparable increase in tear meniscus height has been shown between FNLDO and PANDO groups and successful DCR surgery reduced the severity of epiphora and social embarrassment in both the groups to similar extent.2
In this study 20 eyes in external DCR group, the mean Munk score was 3.8 before intervention and at the 6 month follow-up mean Munk score was 0.35. Out of 34 eyes in injection Botulinum group mean Munk score was 3.85 before intervention where as mean Munk score in this group was 0.78 at the 6 month follow-up. The Munk score before and after intervention was statistically significant, p<0.05, which shows there was improvement in epiphora in both groups. Similar Munk scoring was done in a study conducted by Kaynak et al7 where they have compared the efficacy of injection Botulinum toxin and C-DCR in proximal lacrimal system. The mean Munk score of patient in C-DCR group was 4 before surgery and the mean Munk score was statistically significant on tenth day, first, third, sixth months(1.83,1,1.22 and 1.5 respectively) (p<0.0001)when compared with values before the operation. In patients who were injected Botulinum toxin in the lacrimal gland, the mean Munk score was 3.95 before injection. The improvement of epiphora was also statistically significant on each visit where the mean Munk score were 1.6 on the tenth day, 1.05 at first month, 1.36 at third month and 1.6 at sixth month (p<0.0001)
In this study all the 54 eyes showed retention of dye in FDDT before intervention where as at 6 month follow-up, 19(95%) eyes showed no retention in external DCR group and 31(91.17%) eyes showed no retention of dye in injection Botulinum toxin group. FDDT is a rapid, non-invasive diagnostic test with 95% specificity in diagnosing PANDO. Its sensitivity and specificity for functional epiphora is unknown. A positive FDDT cannot differentiate between anatomical and functional obstruction/lacrimal pump failure. Combining FDDT with a more specific test like syringing, and/or imaging may result in higher sensitivity.2
In our study over all success rate at 6 months after surgery for external DCR is 95% which was similar to study done by O’Donnell et al14 where they reported success rate of 94% for patient who underwent external DCR for patent lacrimal system with average follow up duration of 9.6 weeks. The overall success rate of external DCR for treatment of functional nasolacrimal duct obstruction was 76.9% in a study by Simsek et.al which is markedly lower than approximately 98% successful outcome of ext-DCR for primary nasolacrimal duct obstruction. They grouped the cases into pre-sac and post-sac obstructions according to lacrimal scintigraphy findings. The aim of surgery was to overcome the inflammatory process in the canalicular system in pre-sac where as in post-sac obstructions it was to decrease the distance from puncta to the nasal mucosa. This relatively lower successful outcome in functional obstructions is probably because of the ongoing idiopathic inflammatory process responsible for the obstruction or other factors contributory to epiphora.1 Sahlin and Rose18 reported marked improvement or cure of symptoms in 50% of patients with symptomatic epiphora and patent tear ducts with at least two year follow-up after DCR. Peter and Pearson19 reported 63% success after an average of 11 months of follow-up for 46 ext-DCR with silicone intubation in patients with epiphora and clinically patent lacrimal systems. Delaney and Khooshabeh16 performed ext-DCR with silicone tube intubation in freely patent systems and reported their success rate as 84%(91% for post sac, 67% for pre sac delays) 3-4 months postoperatively. However this rate declined to 70% (80% for post sac and 47% for presac delays) at 3 years.
And the over all success rate for injection Botulinum group was 91.17% in our study which was higher than the over all outcome of 86% reported in a study conducted by Whittaker et.al. Objective evidence of benefit was demonstrated by the change in Schimer test measurements from baseline in over 70% of patients. However, there was a poor correlation between the subjective epiphora scores and the Schirmer test results.7 In our study all 34 eyes who received Botulinum injection received single dose of 5 units among which the 3 eyes showed improvement for only 10-12 weeks. And rest 31 eyes did not require any repeat injection till 6 months followup.1 out of 3 eyes, opted for Dacryocystorhinostomy surgery and rest 2 decline for repeat injection or DCR surgery. Kaynak et al8 reported in their study,13 out of 20 patients had 6-8 months follow-up and did not require reinjection of Botulinum toxin for proximal nasolacrimal duct obstruction in this duration where as 7 patients had 24-53 months follow-up out of which 2 patients requested repeated injections. They had received 4 units of Botulinum injection in lacrimal gland. Botulinum injection was repeated four times in one eye and twice in one eye as a result of patient’s high satisfaction with the treatment.
In our study out of 54 eyes, post-operative complication occurred in 1 (5%) eye in External DCR group where as 10(29.41%) eyes developed post-operative complications in injection Botulinum group. Among 20eyes in External DCR group,1(5%)eye had bleeding as post-operative complication where as out of 34 eyes in injection Botulinum toxin group 10(29.41%) eyes had dry eye at the end of the 6 months follow-up. Among 10 eyes who developed dry eye,1(2.94%)eye also had diplopia for 3 weeks duration, 1(2.94%)eye had subconjunctival hemorrhage and 2(5.88%)eyes had ptosis as early complications which resolved by 4weeks of duration. The post-interventional complications between two groups was statistically significant with p-value <0.05 i.e more number of complications were seen in injection Botulinum toxin group. Whittaker et al6 also reported similar side effects in patients who received 5 units of Botulinum injection for functional epiphora.1 patient developed ptosis 2 days post injection which resolved by 4 weeks and 1 patient reported vertical diplopia for 3 weeks post injection and side effects were reported by patients who received higher dose (5 units) of Botulinum injection. No patient who received a dose of 2.5 units of Botulinum toxin reported any side effects. There was no clinical evidence of dry eyes in any patient. More number of complications occurred in our study in injection Botulinum group may be because of the high dose of Botulinum toxin (5units).Kaynak et al8 reported Blepharoptosis as complication in 5(25%) cases out of 20 which received injection Botulinum toxin 4 units for proximal naso-lacrimal duct obstruction. Two of them who had ptosis >1mm were prescribed apraclonidine hydrochloride 0.5% drops to manage ptosis during the resolution period which was 2-3 weeks.
So injection Botulinum toxin can be considered as an alternative management in case of functional epiphora for patient who do not want to undergo surgical intervention as it avoids the risks and complications of an invasive surgery and general anesthesia. Another advantage of injection is it can be performed in an outpatient clinic.
Conclusion
This study showed that injection Botulinum toxin has equally comparable success rate in the management of functional epiphora. As DCR is an invasive procedure that involves surgical expertise, costs and theatre time .Injection Botulinum is relatively inexpensive and non-invasive with well-tolerated side effects. However it only provides temporary relief to most of the patients and repeated injections are required to the one having significant symptoms. So the advantage of both procedure should be carefully discussed with patients for their optimum satisfaction.
Limitation
This is non-randomized study with small number of sample size 45 patients (54 eyes) only. The study lacks preoperative evaluation of patients with imaging techniques as in some cases only clinical evaluation alone fails to provide conclusive diagnosis where the imaging plays important role. This study has a short follow up duration of 6 months only.