Introduction
Stevens-Johnson-Syndrome (SJS) and Toxic-Epidermal-Necrolysis (TEN), are acute inflammatory diseases of skin and mucous membranes predisposing patients to life-threatening complications like sepsis, respiratory and multi-organ dysfunction.1 After acute-stage subsides, cicatrization of ocular surface progresses, visual impairment and ocular discomfort develops.2, 3, 4 In the acute phase of SJS-TEN, 75-80% patients have ocular involvement. Among these, chronic ocular manifestations develop in 21-29% of pediatric cases and 27-59% of adult cases.
Most frequent ocular sequelae is Dry Eye.5, 6 SJS is defined when skin and mucous membrane involvement is less than 10% , TEN when over 30% and ‘‘overlapping SJS-TEN’’ when 10% to 30%.7
At chronic stage, with identical ocular findings, its difficult to differentiate SJS from TEN. So, ocular surface diseases are collectively termed ‘‘SJS’’ from Ophthalmologist’s perspective.
Chronic stage is characterized by posterior lid margin keratinization and corneal changes that impair vision.
Treatment option for posterior lid margin keratinization include topical all-trans retinoic acid, autologous mucosal membrane grafting, and protective scleral contact lenses. The topical all-trans retinoic acid and autologous mucosal membrane grafting decrease the extent of lid margin keratinization. Topical all trans retinoic acid is a non-invasive means to treat keratinization by altering epithelial cell differentiation. In autologous mucous membrane grafting, surgical excision of the keratinized lid margin and replacing it with mucosal membrane grafted from the oral cavity is required. The scleral lens forms a protective barrier and seals the tear film layer for the corneal surface and help in reducing the extent of mechanical injury to the cornea from the posterior eyelid margin, districhiasis, trichiasis, and other adnexal changes.
In Meibomian gland dysfunction with reduced tear production, treatment options are, artificial tears that supplement natural tear production,8 punctal occlusion that prevents drainage of naturally formed tears and salivary gland transplantation in superior and inferior conjunctival fornices.
In this case report we will observe the manifestation of dry eye associated with Steven Johnson Syndrome, the treatment provided and various treatment options available.
Case Report
A 47 year old male presented to the ophthalmology outpatient department with the chief complaint of diminution of vision, feeling of dryness, grittiness and nonspecific ocular discomfort in both eyes since last 21 years.
He gave history of taking anti-malarial drugs 21 years back after which he developed severe allergic reaction all over his body including both eyes. For this he got admitted and treated in a hospital setup.
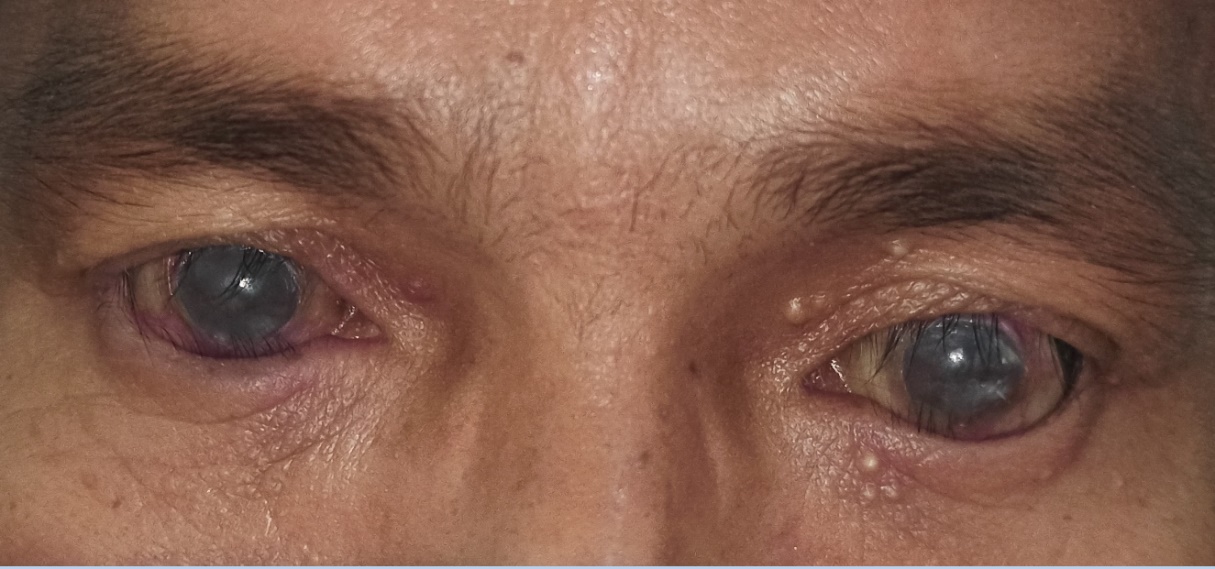
Ocular examination revealed Entropion and Trichiasis of eyelids of both eyes (Figure 1), Conjunctival xerosis and Symblepheron due to cicatrization and Corneal xerosis and keratinization of both eyes (Figure 2).
Both punta of both eyes are found to be stenosed. On General examination – systemic findings were normal and no skin lesions were seen at the present stage of the disease.
Routine blood investigations, blood sugar levels, viral serology, chest x-ray and x-ray of limbs and joints were done, to identify any disease if present for which patient might require drugs that can lead to Steven Johnson Syndrome.
Drugs causing SJS are as follows– Anti malarials (Chloroquine), Anti-gout medication (Allopurinol), Anticonvulsants (Phenytoin, Carbamazepine), Antipsychotic (Haloperidol), Antibiotics (sulphonamides), etc.
The following specific tests for dry eye were done;
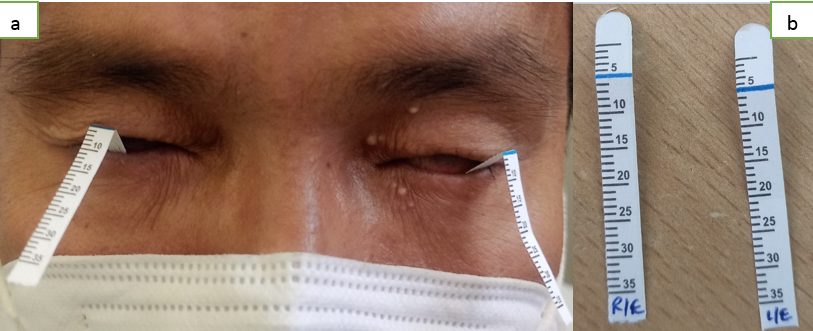
Schirmer test (Figure 3 a and b): R/E - No wetting at the end of 5 min, L/E - No wetting at the end of 5 min
Tear film breakup time: R/E - No tear film present, L/E - No tear film present
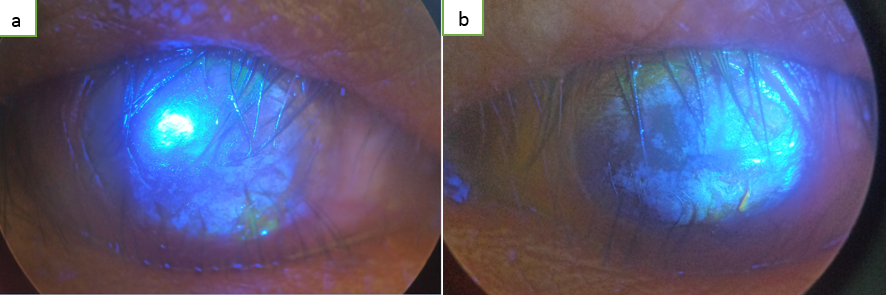
Ocular surface staining (Fluorescein) (Figure 4 a and b): R/E - Stain negative corneal opacity, L/E - Stain negative corneal opacity.
The patient was treated with–
E/D cyclosporine – 1 DROP 2 TIMES DAILY B/E
E/D carboxymethyl cellulose 1% GEL – 1 Drop 4 times daily B/E.
Emollient eye gel –To apply locally at bed time B/E.
Figure 2
Conjunctival xerosis and Symblepheron due to cicatrization and Corneal xerosis and keratinization of both eyes seen in a case of SJS

Discussion
Very severe dryness of the ocular surface causes eye pain, photophobia, foreign body sensation, and visual disturbance, and patients have difficulty in opening their eyes.9 Sometimes, SJS patients present to us with the complaint of severe dryness of the eye despite frequent instillation of artificial tears eye drops.
So, it is necessary to understand that severe dry eye with the combined mechanisms of aqueous tear deficiency, decreased corneal surface wettability, and increased evaporation may be involved in cicatrized cases with Steven Johnson Syndrome.
The initial ocular pathogenesis of Steven Johnson Syndrome is conjunctival inflammation and necrosis. Followed by subsequent destruction of goblet cells and keratinization. Final outcome is often scarring. Mucus production from goblet cells is essential for maintaining the adequate tear film required for corneal clarity. The long-term sequelae occur as a combined effect of cicatricial conjunctivitis and inadequate tear film.
The eyes in which the superior and inferior punctum are occluded due to scarring or surgery (e.g., punctal plugs or cauterization), tear deficiency is often underestimated when the meniscus is first observed. SJS related complications like trichiasis, cicatricial entropion, and scarring of the mucocutaneous junction (lid margin) can be the cause of blink-related microtrauma, and intensify the symptoms related to dry eye.4, 5, 6
It is to be remembered that a stable tear film over the cornea is required for consistent good vision, and that unstable tear film related to dry eye can result in diminution of vision. In fact, SJS patients at the chronic stage usually complain of decreasing visual acuity, especially in the eye with severe dry eye, depending on the time after blinking. By the use of functional visual acuity (FVA) measurement system, Dynamic visual changes can be continuously measured in a 30-second blink-free period in one eye. Kaido et al.10 examined the Dynamic visual changes in SJS using the FVA system and reported that time related decline of FVA was more in patients with SJS as compared to normal subjects. In addition to the above observation, the visual maintenance ratio (VMR) was found to be markedly lower in patients with SJS as compared to patients with Sjogren syndrome (SS) and normal controls.
To achieve a proper treatment of dry eye in SJS cases, it is vital to pay attention to ocular surface inflammation along with dry eye. In SJS, at the chronic stage, there exists persistent conjunctival inflammation.11 Recently, chronic inflammation in the follicles of eyelashes. The administration of artificial tears is necessary to increase the tear volume, and preservative-free artificial tears are recommended for this purpose. Scleral contact lenses, and newly developed limbal-rigid contact lenses, improve the patients’ visual acuity and reduce symptoms.12
As of now, autologous serum/plasma is being widely used for the treatment of dry eye and/or persistent corneal epithelial defects. The application of a punctal plug or surgical punctal occlusion is also effective in some cases.12 In cases of chronic inflammation, low-dose topical steroids decrease the patients’ symptoms. But, when topical steroids are used, strict attention is to be paid to adverse events like infectious keratitis and the elevation of intraocular pressure.
In our case, as it’s in chronic stage, the treatment initially given was directed to reduce any inflammation if present for which topical cyclosporine was given, and to maintain a tear film we gave topical carboxymethyl cellulose 1%.