- Visibility 337 Views
- Downloads 86 Downloads
- Permissions
- DOI 10.18231/j.ijooo.2021.031
-
CrossMark
- Citation
Ocular manifestations in road traffic accidents
- Author Details:
-
Rani Sujatha M.A
-
Syed Saifullah Bokhari *
Abstract
Aim: Road traffic accidents (RTAs) are the most common cause of polytrauma. This study aims to evaluate the various ocular manifestations in cases of RTAs.
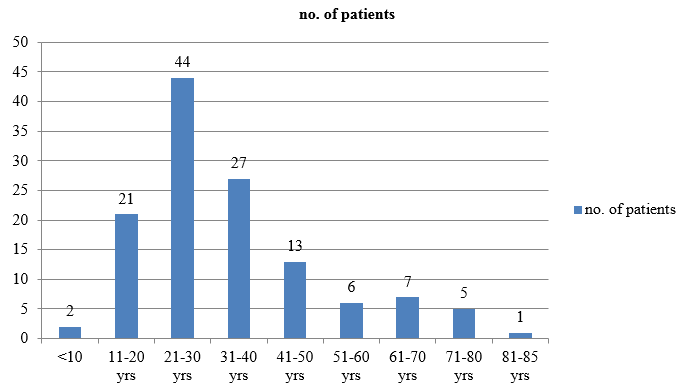
Materials and Methods: A retrospective review of patients who were treated for RTAs in a tertiary hospital in 6 months from December 2018 to May 2019. A total of 126 patients were reviewed. Age ranged from 2 to 85 years. The mean age was 32 years.
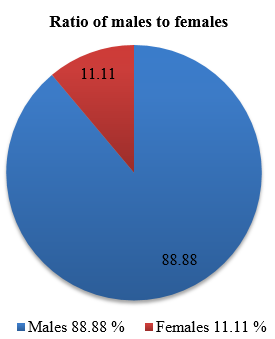
Results: Ophthalmological examination was undertaken in all patients involved in RTA. Out of 126 patients, 112 were males and 14 were females. Young adult males (21-30 years) were most vulnerable to RTAs. Soft tissue injuries were the most common manifestations (57.93%) followed by neuro-ophthalmic manifestations (26.98%) and orbital fractures (15.07%). The presence of CT abnormalities especially intra cranial haemorrhage was associated with neuro-ophthalmic deficits.
Conclusions: Soft tissue injuries were the most common ocular manifestations. It was found that head trauma causes many neuro-ophthalmic manifestations. Relative afferent pupillary defect (RAPD) was the most common neuro-ophthalmic manifestation. The most common cranial nerve involved was found to be oculomotor nerve. Retrobulbar neuritis was a rare finding.
Introduction
Ocular trauma is the cause of blindness in more than half a million people worldwide and it is often the leading cause of unilateral loss of vision, particularly in developing countries.[1] The role of ocular injuries due to head trauma in the causation of blindness and overall prognosis of patients has become a subject of immense importance with RTAs being the most common risk factor.[2] Head injuries are frequently associated with ophthalmic manifestations and consequent visual morbidity.[3] Ocular trauma can be easily prevented by use of various safety precautions. This study aims in providing information on the pattern & magnitude of ocular injuries following RTAs at Dr.B.R.Ambedkar Medical College and Hospital.
Materials and Methods
A retrospective chart review of patients who were involved in RTAs in Dr.B.R. Ambedkar Medical College in 6 months from December 2018 to May 2019. A total of 126 patients were reviewed.
Detailed history regarding the injury was taken and the clinical details were entered into a standard clinical proforma. Uncooperative patients were excluded from the study.
Ophthalmological examination was done at two stages. Bedside examination on admission and evaluation in outpatient department after patient was ambulatory. Bedside examination included extra orbital injury assessment, pupillary response by torchlight, vision by counting fingers at 2 meters distance bedside, extra ocular movement examination, visual field assessment by finger confrontation and fundus examination using direct ophthalmoscope.
Evaluation in out patient department included assessment of visual acuity with pinhole using snellen’s chart, anterior segment evaluation was done with slit lamp. Posterior segment assessment was done on dilated eye by direct and indirect ophthalmoscopy. Intraocular pressure by Goldmann applanation tonometer was done when needed. Neurological visual field defects were assessed using HFA SITA on patients with pupillary involvement and suspected field defect on confrontation. Gonioscopy was done if necessary for the case studied. Computed tomography of brain, skull and spine, MRI and B-Scan was taken whenever appropriate
.
Inclusion criteria
Patients of any age
Individuals who were driving or were in the vehicle during accident as passengers
Patients who sustained ocular injuries during the road traffic accidents
Exclusion criteria
Patients who sustained ocular injuries due to domestic trauma
Patients who sustained ocular injuries due to assault
Patients who sustained ocular chemical injuries
Patients who sustained workplace injuries
Microsoft excel sheet was used to tabulate the data. Mean, ratio and percentages of the variables were calculated. The results found were analyzed and significance by p values was calculated using chi square test.
Results
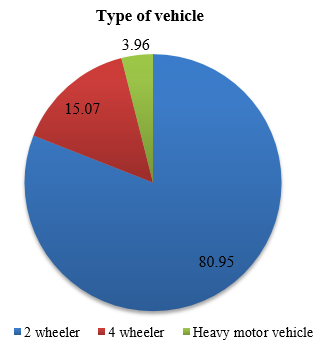
A total of 126 patients were reviewed. Out of these 112 (88.88%) were males and 14(11.11%) were females [[Figure 1]] in the age range of 2-85 years with a mean age of about 32 years [[Figure 2]]. Young adult males were most vulnerable to RTAs. Among the patients 102 (80.95%) were in 2 wheeler, 19(15.07%) in 4 wheeler and 5(3.96%) in heavy motor vehicles [[Figure 3]]. Right eye involvement was seen in 70(55.55%) patients, left eye in 33(26.19%) and both eyes in 23(18.25%).
Soft tissue injuries were the most common manifestation seen in 73 patients (59.93%) followed by neuro-ophthalmic manifestations in 34 patients (26.98%), and orbital fractures in 19 patients (15.07%). The most frequent soft tissue injuries were periorbital ecchymosis in 55 patients (43.65%). Subconjunctival hemorrhage was seen in 26 patients (20.63%), lid laceration in 21 patients (16.66%). macular edema in 7 patients (5.55%) and hyphaema in 13 patients (10.31%). Vitreous haemmorhage and retinal detachment was seen in 8 patents (6.34%) and 3 patients (2.38%) respectively. The most frequently seen neuro-ophthalmic manifestation was relative afferent papillary defect (RAPD) seen in 34 patients (26.98 %) followed by extraocular movement restriction (EOM) in 29 patients (23.01%), disc edema in 18 patients (14.48%) and retrobulbar neuritis in 3 patients (2.38%). Among orbital wall fractures, the most common fracture was involving lateral orbital wall in 9 patients (7.14%), 5 patients (3.96%)with medial wall, 4 patients (3.17%) orbital floor and 1patient (0.79%) with orbital roof fracture [[Table 1]].
Among the 29 cases of EOM restriction 15 cases had cranial nerve palsy. Most commonly involved was oculomotor nerve seen in 6 patients (4.76%), then abducens nerve in 4 patients (3.17%) followed by trochlear and trigeminal nerve involvement both having 2 cases each (1.58%) and facial nerve with 1 patient (0.79%).
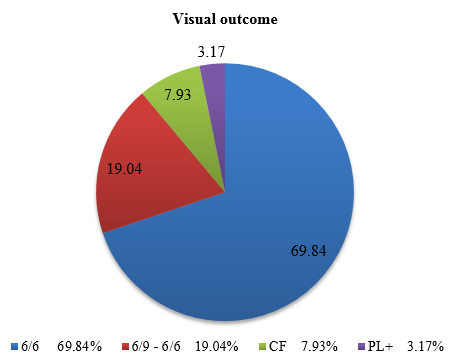
On comparing all the neuroimaging findings of the patients 91 (72.22%) had intracranial haemmorhage (ICH). In 35 patients (27.77%), neuroimaging was normal. In this study 88 patients (69.84%) had visual outcome of 6/6, 24 patients (19.04%) had outcome of 6/9-6/60, 10 patients had visual outcome of CF (counting fingers) and 4 had PL+(perception of light) [[Figure 4]].
|
Type of injury |
n (Percentage) |
|
A. Soft tissue injury |
73 (57.93%) |
|
1. Subconjunctival haemmorhage |
26 (20.63%) |
|
2. Periorbital ecchymosis |
55 (43.65%) |
|
3. Lid laceration |
21 (16.66%) |
|
4. Hyphaema |
13 (10.31%) |
|
5. Proptosis |
3 (2.38%) |
|
6. Ptosis |
7 (5.55%) |
|
7. Vitreous haemmorhage |
8 (6.34%) |
|
8. Macular edema |
7 (5.55%) |
|
9. Retinal detachment |
3 (2.38%) |
|
B. Orbital fractures |
19 (15.07%) |
|
1. Lateral wall |
9 (7.14%) |
|
2. Medial wall |
5 (3.96%) |
|
3. Floor |
4 (3.17%) |
|
4. Roof |
1 (0.79%) |
|
C. Neuro-ophthalmic manifestations |
34 (26.98%) |
|
1. RAPD |
34 (26.98 %) |
|
2. EOM restriction |
29 (23.01%) |
|
3. Cranial nerve palsy |
15 (11.90%) |
|
1. Oculomotor nerve |
6 (4.76%) |
|
2. Trochlear nerve |
2 (1.58%) |
|
3. Abducens nerve |
4 (3.17%) |
|
4. Trigeminal nerve |
2 (1.58%) |
|
5. Facial nerve |
1 (0.79%) |
|
4. Disc edema |
18 (14.28%) |
|
5. Retrobulbar neuritis |
3 (2.38%) |
Discussion
In India which is progressing towards more cosmopolitan standards, road traffic accidents play a major role in physical sufferings of young working generation. Head injury being one of the important cause and eyes being frequently involved in most of head injury patients, it has to be ensured that adequate ophthalmic assessment happens on time and treatment is to be delivered accordingly to prevent permanent visual deficit.[4] India accounts for approximately 10% of RTA world wide. In many series worldwide, traffic accident constitutes the leading cause of head injury which is shown in study of Odebode et al,[5] Kulkarni et al,[6] Masila et al,[7] Sabates et al.[8]
A study conducted by Parri Muralidhar et al showed that male patients were more commonly affected than female patients with M: F ratio of 19:1.[9]
Shtewi M EL et al have done a two year study from an Eye hospital in Libya on road traffic accidents and ocular trauma.[10] They reported that out of 248 patients included in their study, 186(75%) were male and 62(25%) were female. Similarly Johnston PB from Northern Ireland reported the incidence as 72.20% in males and 27.80% in females.[11] Arora AS et al have done a similar study from India, Rajasthan and reported the M: F ratio to be 2.5:1.[12]
Right eye injury was more frequent (60%, 24 patients) than left eye (40%, 16 patients), in the study conducted by Parri Muralidhar et al.[9] The visual acuity immediately after the trauma ranged between 6/6 to PL. Most of the patients had VA between 6/9 to 6/36, who had sustained ocular adnexal injury, periorbital fracture, subconjuctival hemorrhage, and echymosis. Drastic fall of VA to hand movements and perception of light had occurred in two patients who sustained dislocation of lens and posterior segment involvement mainly traumatic optic neuropathy. After treatment there is regain of VA to 6/9 in patients who sustained ocular adnexal injury and periorbital fracture. Most of the patients had sustained subconjuctival hemorrhages, ecchymoses and ocular adnaxal injuries rather than penetrating globe injuries involving posterior segment of the eye.
The most common ocular injury in a study conducted by Menon et al[13] was periorbital oedema with ecchymosis (68.6%). These were also the commonest ocular injuries reported by Alam J et al [14] and Kumarasamy et al[15] in their studies but the commonest ocular injury reported by Muralidhar et al[9] was sub-conjunctival haemorrhage followed by echymosis. In present study eye brow laceration (63.9%) and lid laceration (48.2%) were next in the list (Table 2). In the same study by Kumarasamy et al, the author reported hyphaemia in 4.16% patients, however present study showed only 2.1% of hyphaema.[15]
Patients with neuro-ophthalmic deficit following head trauma can be a diagnostic and therapeutic challenge mostly due to the frequently vague nature of their visual complaints and their coexistent neurologic deficits. Pupil size and reaction to light is very important in the initial assessment of head injury cases. Apart from pupillary signs of uncal herniation and associated primary injuries to the globe, the ocular findings are of secondary importance during emergency management of the patient.[6]
Early signs of temporal herniation include ipsilateral miosis due to oculomotor nerve irritation that is Hutchison’s stage I which is followed by paresis causing ipsilateral pupillary dilatation and a sluggish response to light that is Hutchison’s stage II. Progressive dilatation of the ipsilateral pupil and miosis of the contralateral pupil which is Hutchison’s stage III and it shows progressive IIIrd nerve palsy due to temporal lobe herniation. This is followed by bilateral dilation of the pupil called Hutchinson’s stage IV.
Moster et al[16] reported III cranial nerve palsy in 30%, IV cranial in 26% and VI cranial nerve palsy in 22% cases. Mariak, after brain autopsy in 12 patients, found serious cranial nerve involvement in 75% of the fatal closed head injury cases.
Kowal’s[17] study reported problems of poor accommodation with one or more cases, convergence insufficiency or acquired pseudomyopia in 36%, vitreoretinal disturbances in 5.6% and vitreous haemorrhages in 3.7% patients. There was one case each of a macular hole, retinal tear and retinal detachment and the one patient who developed bilateral idiopathic blepharospasm also had unexplained diplopia. Ptosis without any evidence of oculomotor nerve palsy or lid or orbital damage was present in 2.5% cases.
Commonly reported abnormalities by Moster et al[16] were, traumatic optic neuropathy (18% as opposed to 2.38% in our study), homonymous hemianopia (15%) and Horner’s syndrome (7%) and multiple abnormalities (42%). Cortical blindness was reported in 0.4–0.6% by Banks et al.[18]
The mechanism of injury for optic neuropathy can be direct, indirect, or due to swelling of optic disc. Contusion injuries to the optic nerve are common after a head injury. An amaurotic pupil is objective proof of an afferent lesion in the pupillary reflex (or a conduction defect in the optic nerve), while at the same time the motor limb (of the third cranial nerve) is intact. It implies that a total and irrecoverable loss of vision has occurred in the affected eye although the optic nerve head may appear normal on first examination in the hospital. Countercoup contusion to the optic nerve has been reported to be transmitted through the temporal bone.[19]
Pupillary signs are of huge importance in indicating the site and severity of injury and in the prognosis of head injury. These help in localizing the site of supratentorial injuries, extradural and subdural haemorrhages, and pontine lesions and various other cranial abnormalities. Hutchison’s pupillary signs indicate progressive coning and the need for emergent life-saving intervention if and when required. Pupillary abnormalities, papilloedema, and lateral rectus palsies usually point towards a poorer outcome. Identifying these early would definitely reduce the incidence of consequent morbidity and mortality and can also help in saving a life.
Kulkarni et al[6] came to the observation that pupillary abnormalities (6.5%), papilloedema (5.5%) and lateral rectus palsy pointed towards a poorer outcome. The presence of eye signs did not mean that a patient was more likely to have neurodeficit. Association between the ocular signs and the outcome was significant (P value = 0.003). All the patients that died had ocular involvement and 13% of patients with ocular signs died. In this study, patients with eye signs of neurological significance were more likely to have neurodeficit and to die than those with other eye signs or no eye signs. There is a significant association between neuro deficit and outcome. Neurodeficit was found in all the patients that died which was significant. The outcome is worse in patients with GCS 6–8 with ocular involvement and neurodeficit (P value = 0.001 - Fisher’s exact test), and those with GCS 11–12 and ocular signs (P value = 0.04). This showed that GCS contributed significantly to the outcome. Neurodefecit and other ocular signs also play a significant role in contributing to the visual outcome and overall outcome of the patient.
Menon et al[13] came to the observation that periorbital edema with ecchymosis was the commonest type of injury occurring in 131(68.6%) of the ocular injuries followed closely by eyebrow laceration occurring in 122(63.9%) and lid laceration in 92(48.2%) patients with ocular injuries. Out of the 191 ocular injuries, 186(97.38%) were closed globe injuries and 5(2.6%) were open globe injuries. Traumatic optic neuritis was the commonest posterior segment injury 12(6.3%). While vitreous or retinal haemorrhage was the commonest posterior segment injury (2.09%). They also observed that 4% sustained ocular injuries while travelling in two-wheelers and 18% injuries occurred while travelling in four-wheeled vehicles.
Sharma et al[20] found that the most common age group involved was, 21–40-year-olds (67.40%). Out of 594 patients, ecchymosis was found in 51.85%, subconjunctival hemorrhage in 44.44%, lid edema in 41.48%, lacerated wound in 22.59%, pupillary involvement in 21.04%, ptosis in 6.73%, cranial nerve palsy in 11.62%, orbital fractures in 10.44%, optic nerve trauma in 4.04%, and exposure keratitis in 4.21%. Patients with bilaterally dilated or pinpoint fixed pupils had a 10 times higher risk of mortality than patients without pupillary involvement. Third nerve involvement was seen 2.85 times more frequently in frontal and parietal region injuries compared to other sites of injury. The involvement of the sixth nerve occurred 4.6 times more frequently in parietal region injuries compared to other sites of injury.
The incidence of abducens nerve palsy in Odebode et al[5] study was reported to be 27% and Abbasi et al[21] study was found to be 41%. But in our study oculomotor nerve was the most common involved with 4.76%. Retrobulbar neuritis was found in 6.5% of the patients in Abbasi et al study compared to 2.38% in our study. In Kumari et al[22] study disc edema was found in 16.27% compared with 14.28% in our study. Similarly lateral wall orbital fractures were the most common orbital fractures in Kumari et al study with 5.81% compared with our study with 7.14%. In Rupani et al[23] study. Maurya et al reported floor and roof of orbit as most commonly fractured orbital wall[24] and Abbasi et al[21] study frontal bone fracture was the most common. Maurya et al[25] [25] observed cranio-orbital trauma in 19.23% cases and cranio-orbitofacial trauma in 25.0% RTA cases
Conclusion
Soft tissue injuries, orbital fractures and neuro – ophthalmic manifestations are the major ocular manifestations in RTAs. Almost all the ocular injuries in RTAs are associated with head injuries. So every patient with head injury should be examined for eye signs on both the first presentation and follow up visits. Visual prognosis will significantly be improved if there is prompt diagnosis and treatment of the patients. Proper examination of the patient is absolutely required with various imaging techniques.
Increasing public awareness of safety precautions is crucial to prevention of RTAs. Many RTAs can occur while driving under the influence of alcohol. Proper checks and awareness should be done to avoid drinking and driving. Proper safety rules should be followed by the public. Safety equipment like wearing helmets which is made mandatory should be followed. Meticulous observation of traffic rules is absolutely necessary. Maintaining the speed limits especially on the highways is very important.
Driving recklessly not only endangers the life of the person driving but also the passengers in the vehicle and also others outside the vehicle which may be other drivers or even pedestrians.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- McCann J, Seiff S. Traumatic neuropathies of the optic nerve, optic chiasm, and ocular motor nerves. Curr Opin Ophthalmol. 1994;5(6):3-10. [Google Scholar] [Crossref]
- Baker R, Epstein A. Ocular motor abnormalities from head trauma. Surv Ophthalmol. 1991;35(4):245-67. [Google Scholar] [Crossref]
- Thurman DJ, Jeppson L, Burnett CL. Surveillance of traumatic brain injury in Utah. West J Med. 1996;165:192-6. [Google Scholar]
- Kumari R, Saha B, Saha K. Ocular manifestations in head injury patients - A prospective Study. Int J Comtemporary Med Res. 2017;4(8):1648-51. [Google Scholar]
- Odebode TO, Ademola-Popoola DS, Ojo TA, Ayanniyi AA. Ocular and visual complications of head injury. Eye. 2005;19(5):561-6. [Google Scholar] [Crossref]
- Kulkarni AR, Aggarwal SP, Kulkarni RR, Deshpande MD, Walimbe PB, Labhsetwar AS. Ocular manifestations of head injury: a clinical study. Eye. 2005;19(12):1257-63. [Google Scholar] [Crossref]
- Masila F, Kiboi J, Marco S, Njuguna M. Ocular findings in patients with head Injury. J Ophthalmolgy Eastern, Cent Southern Afr. 2014;18(2). [Google Scholar]
- Sabates N, Gonce M, Farris B. Neuroophthalmological findings in closed head trauma. J Clin Neuro-ophthalmol. 1991;11:273-7. [Google Scholar]
- Muralidhar P, Chowdary NL. Ocular manifestations in road traffic accidents: a study done at a medical college hospital in South India. Int J Contemp Med Res. 2016;3(8):2337-9. [Google Scholar]
- Shtewi ME, Shishko MN, Purohit GK. Road Traffic Accidents and Ocular Trauma: Experience at Tripoli Eye Hospital, Libya. Community Eye Health. 1999;12:11-2. [Google Scholar]
- Johnston PB, Armstrong MF. Eye injuries in Northern Ireland two years after seat belt legislation.. Br J Ophthalmol. 1986;70(6):460-2. [Google Scholar] [Crossref]
- Arora AS, Bhargava G, Chauhan A, Singh P. Ocular trauma in road traffic accidents: Experience at Mathura Das Hospital. Rajasthan J Ophthalmol. 2011;3:1-3. [Google Scholar]
- Menon L, Mani S, Mathew A. The prevalence of ocular manifestations in road traffic accidents treated at a rural tertiary care hospital in south india: a cross sectional study. Int J Res Med Sci . 2017;5(10):4380-4. [Google Scholar] [Crossref]
- Alam J, Bhattacharjya H, Roy A, Das M. Epidemiology and outcome of ocular trauma among the road traffic accident cases attending a tertiary care hospital in Tripura. Int J Med Sci Public Health. 2014;3(4):422-4. [Google Scholar] [Crossref]
- Kumarasamy R, Velpandian U, Anandan H. Visual outcome in ocular injuries in road traffic accident. Int J Sci Stud. 2016;4(5):151-3. [Google Scholar]
- Moster ML, Volpe NJ, Kresloff MS. Neuro-ophthalmic findings in head injury. Neurol. 1999;52(2). [Google Scholar]
- Kowal L. Ophthalmic manifestations of head injury. Aust New Zealand J Ophthalmol . 1992;20(1):35-40. [Google Scholar] [Crossref]
- Banks M, Lessell S. Neuroophthalmology and Trauma. Int Ophthalmol Clin. 2002;42(3):1-12. [Google Scholar] [Crossref]
- Smith JL. Some neuro-ophthalmological aspects of head trauma. Clin Neurosurg. 1966;13:181-96. [Google Scholar]
- Sharma B, Gupta R, Anand R. Ocular manifestations of head injury and incidence of post-traumatic ocular motor nerve involvement in cases of head injury: a clinical review. Int Ophthalmol. 2014;34:893-900. [Google Scholar]
- Abbasi K, Raza A, Qadeer B. Ocular manifestations associated with head injury. Pak J Ophthalmol. 2016;32(2):111-6. [Google Scholar]
- Kumari R, Saha B, Saha K. Ocular manifestations in head injury patients - A prospective Study. Int J Comtemporary Med Res. 2017;4(8):1648-51. [Google Scholar]
- Rupani R, Verma A, Rathore S. Patterns of skull fractures in cases of head Injury by blunt force. Acad Forensic Med. 2013;35:336-8. [Google Scholar]
- Maurya RP, Jain P, Singh VP, Singh MK, Mishra CP, Verma A. Etiology and pattern of orbital fractures in a teaching hospital. IP Intern J Ocul Oncol Oculoplast. 2017;3(3):184-92. [Google Scholar]
- RM, VS, CM, PJ, AK, MP. Eye injuries in motor vehicle accidents: Epidemiology, spectrum of injury and analysis of risk factors. IP Int J Ocul Oncol Oculoplasty. 2021;7(1):30-9. [Google Scholar]
How to Cite This Article
Vancouver
M.A RS, Bokhari SS. Ocular manifestations in road traffic accidents [Internet]. IP Int J Ocul Oncol Oculoplasty. 2021 [cited 2025 Oct 19];7(2):157-162. Available from: https://doi.org/10.18231/j.ijooo.2021.031
APA
M.A, R. S., Bokhari, S. S. (2021). Ocular manifestations in road traffic accidents. IP Int J Ocul Oncol Oculoplasty, 7(2), 157-162. https://doi.org/10.18231/j.ijooo.2021.031
MLA
M.A, Rani Sujatha, Bokhari, Syed Saifullah. "Ocular manifestations in road traffic accidents." IP Int J Ocul Oncol Oculoplasty, vol. 7, no. 2, 2021, pp. 157-162. https://doi.org/10.18231/j.ijooo.2021.031
Chicago
M.A, R. S., Bokhari, S. S.. "Ocular manifestations in road traffic accidents." IP Int J Ocul Oncol Oculoplasty 7, no. 2 (2021): 157-162. https://doi.org/10.18231/j.ijooo.2021.031
