Introduction
Uveal melanoma is most frequent primary intraocular tumor in adult. It affects mostly (97.8%) Caucasian race, particularly whites of northern European descent and rather rare among Indians and blacks.1 Uveal melanoma is the second most common type of primary melanoma after cutaneous melanoma, comprises of 3-5% of all melanomas.2 Symptoms of uveal melanoma depends on the location of the primary tumor. About 40-50% of patients with primary uveal melanoma ultimately develop systemic metastasis.3 Most common site of systemic metastasis is liver (95%) followed by lung (46%), bone (29%) and skin (17%).3, 4 The reported five-year survival rates after diagnosis of uveal melanoma is 45%.5 Most common type of primary uveal melanoma is choroidal melanoma. Ciliary body melanoma is rare and patient usually present late in advanced stage due to hidden location. We emphasis the role of careful clinical examination, fundus examination and investigation in asymptomatic patients so that disease can be diagnose early before metastasis.
Case Report
A 70 year old male patient presented to the out patient department of Sankara Eye Hospital, Kanpur with chief complaints of gradual progressive diminution of vision in right eye since 2 years. There was no significant medical and family history, no history of eye injury or any previous eye surgery.
On examination right eye visual acuity was finger count, left eye vision was 6/18. Pupillary reaction was ill sustained in right eye while it was normal in left eye. There relative afferent pupillary defect was not elicitable in right eye. Extraocular muscle movement was normal in both eyes in all gazes. On slit lamp examination right eye congestion and few dilated episcleral vessels were seen. The cornea was clear and anterior chamber was shallow in the inferior half. A dark brown colored, inferotemporal mass was seen behind the iris (Figure 1).There was a posterior subcapsular cataract in inferior quadrant of the lens. Left eye examination was with in normal limit except early lental changes. Intraocular pressure was 14 mmHg in both eyes by applanation tonometer.
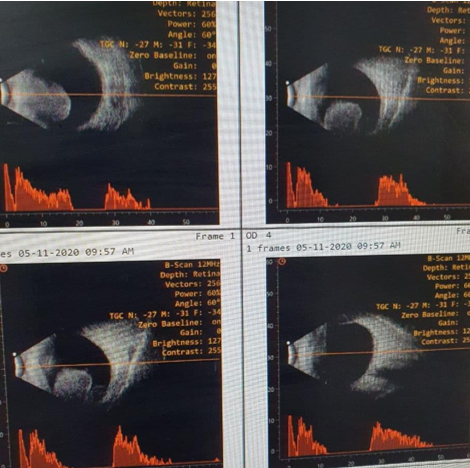
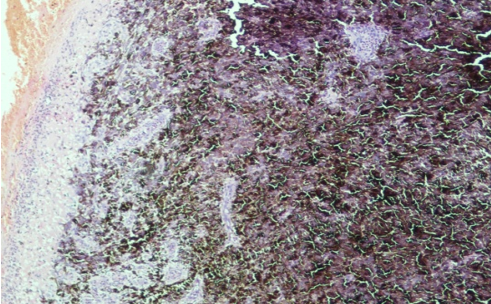
On fundus examination of right eye, we were not able to visualize inferior retina while rest optic disc and retinal vessels were normal. In left eye fundus examination no abnormality was detected. On indirect examination in right eye a protruding ciliary body mass dark brown in color straddling. On the basis of clinical findings a provisional diagnosis of ciliary body melanoma was made and B-scan ultrasonography, OCT and MRI brain with orbit was recommended. B -scan ultrasonography revealed a solid nodular mass in the region of ciliary body of right eye (Figure 2) without any evidence of choroidal lesion or retinal detachment. . OCT images of both eye were normal. Chest X-ray and ultrasonography of abdomen was normal. Patient was referred to ocular oncologist at higher center. Enucleation of the right eye was done in Regional Institute of Ophthalmology, Banaras Hindu University, Varanasi, under local anesthesia with the patient’s consent. Histopathological examination suggestive of mixed cell type of malignant melanoma (Figure 3). Patient was kept under regular follow-up and five months after enucleation patient was alright without any recurrence.
Discussion
Primary uveal melanoma is rare in Indian population and ciliary body melanoma is rather rarer. Etiology remains, unknown. However several predisposing factors has been reported like light iris, light skin, uveal nevus, congenital ocular melanocytotosis and xeroderma pigmentosa etc.6 The hidden location of the ciliary body melanoma makes diagnosis difficult, pupillary dilatation and 3-mirror contact lens are needed to identify the tumor. Transillumination is helpful in localizing the darkly pigmented tumor. Ultrasonography is a useful imaging technique for in eyes with media opacity. Tumors of > 3mm thickness can be accurately diagnosed by A-Scan ultrasonography. USG-biomicroscopy (UBM) helps to estimate the tumor size and to define the anterior border of tumor.6 Ciliary body melanoma can extend locally to iris, retina and transscleral and due to high blood supply can metastasis early to organs like liver and lung.7, 8, 9 Treatment include brachytherapy, iridocyclectomy on the basis of size. Enucleation becomes inevitable because ciliary body melanoma usually advances before getting diagnosed. 10