- Visibility 102 Views
- Downloads 27 Downloads
- DOI 10.18231/j.ijooo.2021.013
-
CrossMark
- Citation
A clinical study of vitamin d supplementation in diabetic retinopathy patients with type 2 diabetes mellitus
- Author Details:
-
Rani Sujatha M.A
-
Ranjitha KC *
Introduction
Diabetes Mellitus continues to be a major health burden all over the world. According to the latest data by the WHO, almost 422 million individuals are estimated to be suffering from diabetes mellitus.[1], [2] The increasing trend towards unhealthy food practices, sedentary lifestyle and physical inactivity can be attributed to this rise in the burden of diabetes mellitus. diabetic retinopathy remains a leading cause of blindness all over the world especially in the working age group with maximum patients presenting in the late stages with significant visual loss due to lack of awareness. Vitamin D deficiency has been implied as a risk factor for development of diabetes mellitus by several studies.[3], [4] Serum vitamin D levels have a role in preventing angiogenesis and reducing pro-inflammatory cytokines thereby implicating a protective role against development of diabetic retinopathy.[5], [6]
Materials and Methods
100 patients with type 2 diabetes melitus and diabetic retinopathy were included in this retrospective study which was carried out at the vitreoretinal services, departmentof ophthalmology at DR B R Ambedkar medical college and hospital over a period of 1 year
Inclusion criteria
Patients aged 40 years and above.
Patients with type 2 Diabetes Mellitus who are diagnosed as non proliferative diabetic retinopathy or Proliferative Diabetic Retinopathy.
Exclusion criteria
Patients with type 1 Diabetes mellitus
Patients previously on vitamin D supplementation.
Patients with vitreous haemorrhage.
Patients with diabetic retinopathy associated with CNVM
History of disorders affecting the metabolism of Vitamin D and illness including renal failure, hepatic dysfunction, and musculoskeletal disorders were excluded.
All patients were screened with a detailed history including nature & duration of symptoms, duration of exposure to sunlight, and diet history.
Ocular examination
Visual acuity was assessed by Snellen’s chart and refractive status was noted
Anterior segment evaluation with slit lamp biomicroscopy was performed
Intraocular pressure was measured using Goldmann Applanation tonometer
Diabetic retinopathy was evaluated by a dilated fundus examination using 90D & indirect ophthalmoscopy
Spectral domain optical coherence tomography
The Diabetic retinopathy was classified as per the ETDRS.
50 patients received weekly oral supplementation of 4000 IU of Vitamin D for a duration of 6 months, constituting the treatment arm, while the other 50 patients served as the control arm.
Results
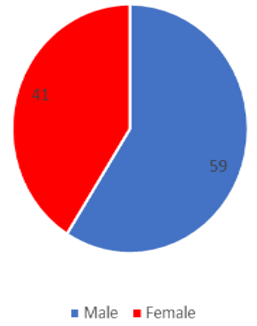
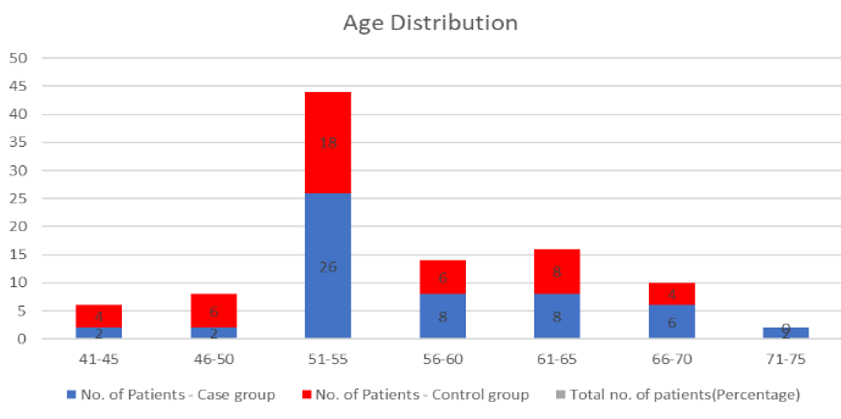
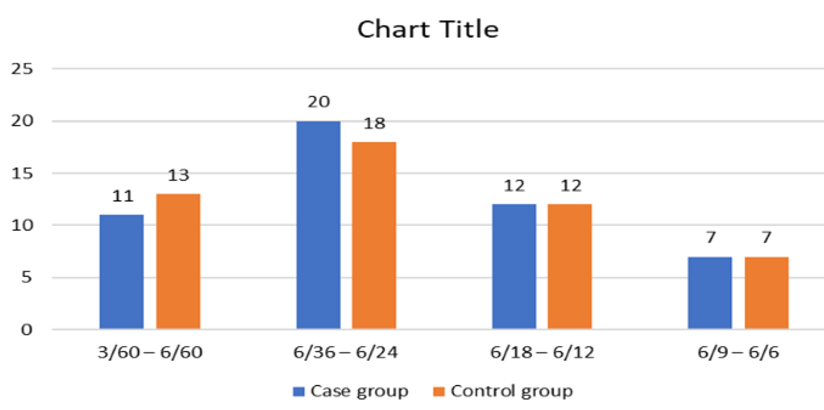
A total of 100 patients were reviewed. Out of these 59 were males and 41 were females [[Figure 1]] in the age range of 41-75 years [[Figure 2]]. 22.62% cases and 24% controls had visual acuity of 3/60-6/60. 40% cases and 36% controls had 6/36-6/24. 24% cases and 24% controls had 6/18-6/12 and 14% cases and 16% controls had 6/9-6/6 [[Figure 3]]. Among the 100 patients enrolled in the study a total
76 patients were vitamin D deficient (<20ng/ml), 15 patients were found to be vitamin D insufficiency (20-30ng/ml), 9 patients were found to have normal vitamin D levels .The mean vitamin D levels at presentation was 23.48ng/ml [[Table 1]].
Mean vitamin D at 6 months among cases was found to be 39.8ng/ml. Mean vitamin D at 6 months among controls was 17.2ng/ml [[Table 2]].
Of the 100 patients 10 patients (20%) had moderate NPDR in cases and 13(26%) in controls and 19(38%) in cases with severe NPDR and 21(48%) in controls. 18(36%) in cases and 14(28%) in controls in very severe NPDR and 3(6%) cases in early PDR and 2(4%) in controls [[Table 3]]. At 3 months, no progression noted in moderate, severe and very severe NPDR. However in control group 20% progressed to high risk PDR which is not found in cases. It was statistically significant (p value < 0.05) [[Table 4]]. At 6 months progression to high risk PDR noted only in 2% of the cases but in 28% controls and even to progression to early PDR was increased to 12% in controls. It was statistically significant (p value < 0.05) [[Table 5]].
|
Serum 25 hydroxy vitamin D levels (ng/ml) |
No. of patients |
|
|
|
|
|
|
Moderate NPDR |
Severe NPDR |
Very severe NPDR |
Early PDR |
Total patients |
|
<20 |
14 |
31 |
28 |
3 |
76 |
|
20-30 |
5 |
6 |
3 |
1 |
15 |
|
30-100 |
4 |
3 |
1 |
1 |
9 |
|
>100 |
0 |
0 |
0 |
0 |
0 |
|
Serum 25 hydroxy vitamin D3 level (ng/ml) in cases at 6 months |
No. of patients |
Percentage |
|
<20 |
2 |
4% |
|
20-30 |
40 |
80% |
|
30-100 |
8 |
16% |
|
>100 |
0 |
0% |
|
Severity of retinopathy at presentation |
Case group |
Percentage in case group |
Control group |
Percentage in control group |
|
Moderate NPDR |
10 |
20% |
13 |
26% |
|
Severe NPDR |
19 |
38% |
21 |
42% |
|
Very severe NPDR |
18 |
36% |
14 |
28% |
|
Early PDR |
3 |
6% |
2 |
4% |
|
High-risk PDR |
0 |
0% |
0 |
0% |
|
Severity of retinopathy at 3 month |
No. of eyes in case group |
Percentage in case group |
No. of eyes in control group |
Percentage in control group |
|
Moderate NPDR |
3 |
18% |
10 |
20% |
|
Severe NPDR |
20 |
40% |
18 |
36% |
|
Very severe NPDR |
17 |
34% |
11 |
22% |
|
Early PDR |
4 |
8% |
1 |
2% |
|
High-risk PDR |
0 |
0% |
10 |
20% |
|
Severity of retinopathy at 6 month |
No. of eyes in case group |
Percentage in case group |
No. of eyes in control group |
Percentage in control group |
|
Moderate NPDR |
6 |
12% |
7 |
14% |
|
Severe NPDR |
18 |
36% |
11 |
22% |
|
Very severe NPDR |
20 |
40% |
12 |
24% |
|
Early PDR |
5 |
10% |
6 |
12% |
|
High-risk PDR |
1 |
2% |
14 |
28% |
Discussion
Diabetic retinopathy remains one of the leading causes of visual loss and after duration of diabetes exceeding 15 years, it affects three out of four diabetic patients. Commonest cause of significant loss of vision in DR is diabetic macular edema.[7] In our study 75% of patients belonged to the 5th and 6th decades of life. This may be due to the fact that prevalence of systemic diseases such as diabetes, increases with increasing age according to Daniel M.Tayloret al. Survey ophthalmology.[8] In the study, 59% males and 41% females were affected with diabetic retinopathy. Although an increased percentage of males were found to be affected, no significant male preponderance was observed. This finding was consistent with previous studies. Among the 100 patients enrolled in the study a total of 76 patients had vitamin D deficient and 15 patients were found to be vitamin D insufficient and 9 patients were found to have normal vitamin D levels.
Aksoy H. et. Al demonstrated that decrease in vitamin D resulted in uncontrolled angiogenesis and neovascularization of retina.[9] A cross-sectional study of type 2 diabetic patients conducted by Suzuki A et. Al. showed a significant association between the existence of proliferative retinopathy and a decrease in 25(OH) D.[10] A study conducted by Joergensen C et al found a decrease in 25(OH) D according to the number of microvascular complications present.[11] A clinic-based, cross-sectional study by Payneset et al. to assess the relationship between vitamin D status and diabetic retinopathy concluded that diabetic subjects, especially those with PDR, have lowered 25(OH) D levels than those without diabetes.[12]
In our study the mean serum 25 hydroxy Vitamin D level of 39.8 ng/ml was attained in the cases following 6 months of oral supplementation, suggesting that this dose used was adequate for normalization of serum vitamin D levels. The mean levels remained deficient (17.2ng/ml) in the controls at the end of 6 month. At 3 months, no progression noted in moderate, severe and very severe NPDR. However in control group 20% progressed to high risk PDR which is not found in cases. It was statistically significant (p value<0.05). At 6 months progression to high risk PDR noted only in 2% of the cases but in 28% controls and even progression to early PDR was increased to 12% in controls. It was statistically significant (p value <0.05).
Conclusion
From the results of this study we can conclude that oral supplementation of Vitamin D in addition to the recommended treatment with photocoagulation, delays the progression of severe, very severe and early PDR. Our study demonstrated that low levels of vitamin D may be a risk marker of development or progression of diabetic retinopathy. It is advisable to conduct ophthalmologic examination at regular intervals in diabetics whose serum 25 hydroxy vitamin D concentrations are diminished. Serum 25 hydroxy vitamin D concentrations could become a useful biochemical marker to predict the severity of DR in patients with diabetes mellitus in the future.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- . World Health Organization,Global Report on Diabetes. Geneva. 2016. [Google Scholar]
- R P Maurya. Diabetic retinopathy: My brief synopsis. Ind J Clin Exp Ophth 2015. [Google Scholar]
- M Baz-Hecht, AB Goldfine. The impact of vitamin D deficiency on diabetes and cardiovascular risk. Curr Opin Endocrin Diab Obes 2010. [Google Scholar] [Crossref]
- SE Judd, V Tangpricha. Vitamin D Deficiency and Risk for Cardiovascular Disease. Am J Med Sci 2009. [Google Scholar] [Crossref]
- X Palomer, JM González-Clemente, F Blanco-Vaca, D Mauricio. Role of vitamin D in the pathogenesis of type 2 diabetes mellitus. Diabetes Obes Metab 2008. [Google Scholar] [Crossref]
- D M Albert, EA Scheef, S Wang. Calcitriol is a potent inhibitor of retinal neovascularization. Invest Ophthalmol Vis Sci 2007. [Google Scholar]
- R P Maurya. Dabetic macular edema: An overview. Indian J Clin Exp Ophthalmol 2019. [Google Scholar] [Crossref]
- DM Taylor. Aphakic cystoid macular edema. Longterm clinical observations. Survey Ophthalmol 1984. [Google Scholar]
- H Aksoy, F Akçay, N Kurtul, O Baykal, B Avci. Serum 1,25 dihydroxy vitamin D (1,25(OH)2D3), 25 hydroxy vitamin D (25(OH)D) and parathormone levels in diabetic retinopathy. Clin Biochem 2000. [Google Scholar] [Crossref]
- A Suzuki, M Kotake, Y Ono, T Kato, N Oda, N Hayakawa. Hypovitaminosis D in Type 2 Diabetes Mellitus: Association with Microvascular Complications and Type of Treatment. Endocr J 2006. [Google Scholar] [Crossref]
- C. Joergensen, P. Hovind, A. Schmedes, H.-H. Parving, P. Rossing. Vitamin D Levels, Microvascular Complications, and Mortality in Type 1 Diabetes. Diabetes Care 2011. [Google Scholar] [Crossref]
- F Payne, R Ray, D G Watson. VitaminD insufficiency in diabetic retinopathy. Endocr Pract 2012. [Google Scholar]
How to Cite This Article
Vancouver
M.A RS, KC R. A clinical study of vitamin d supplementation in diabetic retinopathy patients with type 2 diabetes mellitus [Internet]. IP Int J Ocul Oncol Oculoplasty. 2021 [cited 2025 Sep 11];7(1):64-67. Available from: https://doi.org/10.18231/j.ijooo.2021.013
APA
M.A, R. S., KC, R. (2021). A clinical study of vitamin d supplementation in diabetic retinopathy patients with type 2 diabetes mellitus. IP Int J Ocul Oncol Oculoplasty, 7(1), 64-67. https://doi.org/10.18231/j.ijooo.2021.013
MLA
M.A, Rani Sujatha, KC, Ranjitha. "A clinical study of vitamin d supplementation in diabetic retinopathy patients with type 2 diabetes mellitus." IP Int J Ocul Oncol Oculoplasty, vol. 7, no. 1, 2021, pp. 64-67. https://doi.org/10.18231/j.ijooo.2021.013
Chicago
M.A, R. S., KC, R.. "A clinical study of vitamin d supplementation in diabetic retinopathy patients with type 2 diabetes mellitus." IP Int J Ocul Oncol Oculoplasty 7, no. 1 (2021): 64-67. https://doi.org/10.18231/j.ijooo.2021.013
