- Visibility 98 Views
- Downloads 40 Downloads
- DOI 10.18231/j.ijooo.2021.012
-
CrossMark
- Citation
Abuse of topical steroids in VKC resulting in steroid induced glaucoma in paediatric age group
- Author Details:
-
Shweta. B. Karanvi *
-
Rani Sujatha MA
Introduction
Vernal keratoconjunctivitis (VKC) is bilateral, interstitial, self-limiting allergic inflammation of the conjunctiva having periodic seasonal incidence usually seen in children around 4 to 20 years.[1]
It is mainly type 1 mediated hypersensitivity reaction to pollen allergens usually seen in subjects with a atopic background such as asthma, eczema.[2] More commonly seen in summer hence known as warm weather conjunctivitis presents with a marked burning and itching sensation. Signs can be described in 3 forms palpebral, bulbar and mixed forms.[3]
The treatment of the VKC includes avoiding the causative agents, cold fomentation, mast cell stabilizers, antihistamines, NSAIDS, lubricants. Up to 90% of the subjects require corticosteroids during the course of the disease.[4]
But due to its potency, high effectiveness and early symptomatic treatment corticosteroids are abused without the knowledge of its vision threatening complications mainly cataract and glaucoma. Usually prescribed by pharmacy, general practitioners and quacks without the knowledge of its complications.[5]
Vision loss resulting from cataract is reversible and relatively easy to manage but glaucoma is often recognised late leaving patients with permanent visual impairment.[6]
Current therapy of ocular allergy involves elimination of the offending allergen, modulation of the immune system, and pharmacologic inhibition of the chemical mediators and rebamipide can be effective in VKC with giant papillae not responding to topical steroid.[7], [8]
Materials and Methods
This is a retrospective study conducted from July 2018 to August 2019. 600 children diagnosed with VKC between the age group of 8 to 16 years on treatment for nearly 2 years were included.
Patients using topical steroids like dexamethasone were included in group 1 and Patients using unknown steroids were included in group, based on the history of drug use and coexisting presentation of ocular hypertension it was presumed that it might be steroid for group 2.
The patients who met the 2 out of the 3 following criteria were included in the study: IOP > 21mmHg on more than 2 occasions, Optic nerve head changes due to glaucoma, Visual field defects analyzed by Humphrey automated perimeter. The patients having angle anomaly, history of congenital or developmental glaucoma, Trauma and Uveitis were not taken for the study.
Detailed demographic data about symptoms of marked burning and itching sensation, mild photophobia, lacrimation, stringy discharge and heaviness of lids and History of steroid use including drug name, duration, and frequency and the clinical details were noted down and entered into a standard clinical proforma. Uncooperative patients were excluded from the study.
Ophthalmic examination included, Best Corrected Visual Acuity was done by Snellen’s chart, Slit lamp bio microscopy, Goldman Applanation Tonometry, Fundus examination by indirect ophthalmoscope or 90D lens, Gonioscopy and Visual field defects by Humphreys automated perimeter.
The type of the VKC presentation was noted as palpebral, bulbar and mixed. Palpebral when the upper tarsal conjunctiva of both the eyes was involved giving a cobble stone appearance and the bulbar form when dusky red triangular congestion was present in bulbar conjunctiva with presence of limbal papillae and the mixed form when both bulbar and palpebral conjunctiva was involved
Statistical analysis
Mean, median, standard deviation, ranges were evaluated for continuous variables and for categorical variables, frequency and percentages were recorded. Chi-square test and ANOVA test were also used whenever necessary Independent t test was used to compare mean between the two group. P value of less than 0.05 within 95% CI was considered statistically significant
Results
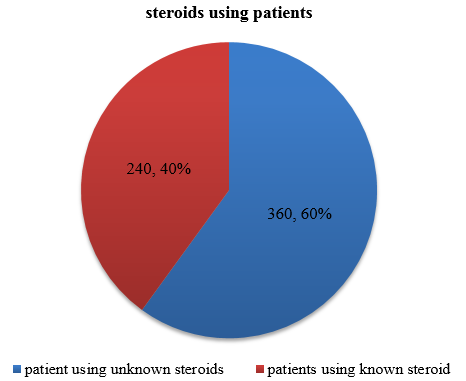
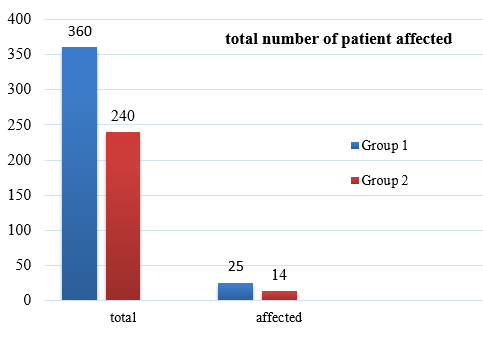
This study included total of 600 patients. It was found that 360 of 600 patients were using unknown steroids, 260 out of 600 were under the usage of known steroids (dexamethasone).
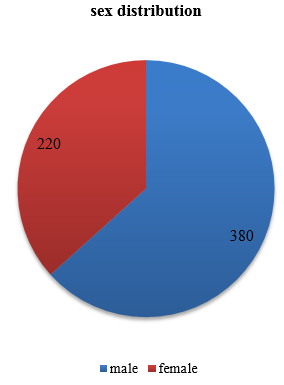
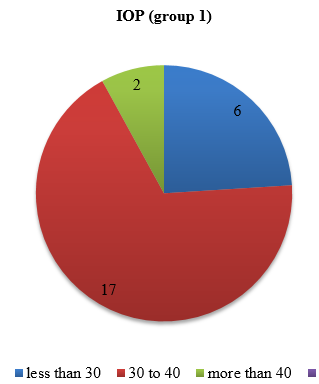
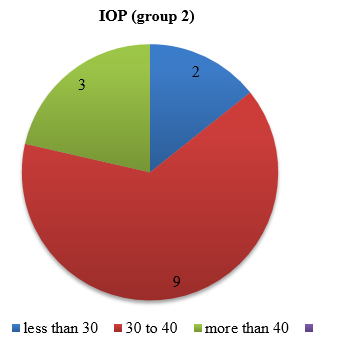
380 out of 600 were male and 220 were female. The duration of usage was 690 and 660 days in group 1 and group 2 respectively. IOP in the group 1 was found to be less than 30 in 6 patients between 30-40 in 17 patients and more than 40 in 2 patients, whereas in group 2 it was found to be less than 30 in 2 patients, between 30-40 in 9 patients and more than 40 in 3 patients.
It was also found that mean cupping in group 1 was 56 ± 0.22 whereas in group 2 it was .48 ± 0.25. the advanced cupping seen in group 1 was 0.75 ± 0.16 and 0.67 ± 0.18 in group 2.
Mean best corrected visual acuity was found to be 0.62 and 0.58 in group 1 and group 2 respectively. Total number of patients affected were 25 and 14 in group 1 and group 2 respectively.
|
Demographic Data |
|
|
Total number |
600 |
|
Patients using topical steroid |
360 |
|
Patients using unknown steroid |
240 |
|
Mean age |
12+-3 yrs. |
|
Best corrected visual acuity (log MAR) |
0.61 |
|
Mean IOP on presentation |
28+-7mmHg |
|
Mean cup disc ratio on presentation |
0.50+-0.33 |
|
S. No |
Parameters |
Group1 |
Group 2 |
|
1 |
Mean days of usage |
650days |
690 days |
|
2 |
IOP Mean |
30+-8mmHg |
32+-6mmHg |
|
3 |
IOP<30mmHg |
6 |
2 |
|
4 |
IOP 30-40mmHg |
17 |
9 |
|
5 |
IOP >40mmHg |
2 |
3 |
|
6 |
Mean cupping |
0.56+-0.22 |
0.48+-0.25 |
|
7 |
Advanced cupping |
0.73+-0.16 |
0.67+-0.18 |
|
8 |
Mean BCVA |
0.62 |
0.58 |
|
9 |
Total number affected |
25 |
14 |
Discussion
This study highlights the visual complications caused by abuse of steroids I children in Indian rural population. We studied children of VKC having raised IOP who were already using topical steroids prescribed somewhere else. These topical steroids were prescribed without counseling the parents or patients about the disease or asymptomatic complications associated with steroid use.
The patients continued to use the steroids, because of the quick relief in symptoms of VKC. Injudicious use of steroids and inadequate monitoring led to steroid induced complications like ocular hypertension, glaucoma and cataract affecting vision markedly
Vision loss resulting from cataract is reversible and relatively easy to manage but glaucoma is often recognized late leaving patients with permanent visual impairment Pradhnya Sen et al, showed that out of 1423 patients, prevalence of steroid induced glaucoma was 3.3% and they concluded that in patients using high potent steroids like dexamethasone and betamethasone have high risk whereas the use of low potency steroid have low risk of steroid induced glaucoma. In our study the prevalence is around 4.16%.[5]
Marcuss ang et al, in their study showed 41(28.3%) out of 145 patients developed ocular hypertension in which 8(5.5%) patients progressed to glaucoma.[5]
Corticosteroid induced IOP elevation is an iatrogenic condition caused by decreased trabecular outflow, usually reversible if the steroid therapy is discontinued earlier but when unrecognised causes primary open angle glaucoma, ultimately leading to glaucomatous optic atrophy which is irreversible.[5]
Vision loss resulting from the cataract is reversible and relatively easy to manage but glaucoma is often recognised late leaving patients with permanent visual impairment.[5]
Conclusion
Steroid induced glaucoma is an important complication seen in patients with VKC due to prolonged use of topical steroids. These children will have long term visual impairment and there will be financial burden to treat complications.[5] Therefore, measures need to be taken collectively by patients, ophthalmologists and the government to prevent steroid misuse. It can be prevented by proper counseling, regular follow up and monitoring the IOP along with visual field testing.
Topical corticosteroids are often used during flare-ups in combination with mast cell stabilizers as maintenance treatment for VKC.[9]
The pathogenesis of VKC is complex and involves environmental, endocrine, racial, and genetic factors.[10] Use of the weak steroids can be helpful for the prevention the disease at the earliest. Thus, the usage of topical steroids without proper consultation or the long term in judicial usage should be avoided. And if the patients are on the therapy regular IOP monitoring along with the monitoring of the above-mentioned parameters should be done so that timely measures can be taken to prevent permanent visual loss
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- H Addis, B Jeng. Vernal keratoconjunctivitis. Clin Ophthalmol 2018. [Google Scholar] [Crossref]
- R P Maurya, V P Singh, M K Singh, P Bhushan, Dr. J. K. Mishra. Ocular Allergy: An Overview Written in Book: Update on Respiratory Disease & Allergy. 2015. [Google Scholar]
- Stefan & Smedt, Philippe Kestelyn. Vernal keratoconjunctivitis: an update. Br J Ophthalmol 2012. [Google Scholar] [Crossref]
- A Leonardi. Management of vernal keratoconjunctivitis. Ophthalmol Ther 2013. [Google Scholar]
- P Sen, S Jain, A Mohan, C Shah, A Sen, E Jain. Pattern of steroid misuse in vernal keratoconjunctivitis resulting in steroid induced glaucoma and visual disability in Indian rural population: An important public health problem in pediatric age group. Indian J Ophthalmol 2019. [Google Scholar] [Crossref]
- SV Bangal, MS Bankar, AJ Bhandari, RK Prasad. Bilateral steroid induced glaucoma in vernal keratoconjunctivitis. Int J Med Res Health Sci 2015. [Google Scholar] [Crossref]
- MB Abelson, K Schaefer. Conjunctivitis of allergic origin: Immunologic mechanisms and current approaches to therapy. Survey Ophthalmol 1993. [Google Scholar] [Crossref]
- L Dorennavar, RP Maurya, VP Singh, MK Singh, K Sharma, R Sharma. The role of Rebamipide ophthalmic suspension in management of dry eye disease. Ind J Clin Exp Ophthalmol 2015. [Google Scholar] [Crossref]
- SD Smedt, G Wildner, P Kestelyn. Vernal keratoconjunctivitis: an update. Br J Ophthalmol 2013. [Google Scholar] [Crossref]
- M D Khan, N Kundi, N Saeed, A Gulab, A F Nazeer. A study of 530 cases of vernal conjunctivitis from the North West Frontier Province of Pakistan. Pak J Ophthalmol 1986. [Google Scholar]
How to Cite This Article
Vancouver
Karanvi SB, MA RS. Abuse of topical steroids in VKC resulting in steroid induced glaucoma in paediatric age group [Internet]. IP Int J Ocul Oncol Oculoplasty. 2021 [cited 2025 Sep 12];7(1):60-63. Available from: https://doi.org/10.18231/j.ijooo.2021.012
APA
Karanvi, S. B., MA, R. S. (2021). Abuse of topical steroids in VKC resulting in steroid induced glaucoma in paediatric age group. IP Int J Ocul Oncol Oculoplasty, 7(1), 60-63. https://doi.org/10.18231/j.ijooo.2021.012
MLA
Karanvi, Shweta. B., MA, Rani Sujatha. "Abuse of topical steroids in VKC resulting in steroid induced glaucoma in paediatric age group." IP Int J Ocul Oncol Oculoplasty, vol. 7, no. 1, 2021, pp. 60-63. https://doi.org/10.18231/j.ijooo.2021.012
Chicago
Karanvi, S. B., MA, R. S.. "Abuse of topical steroids in VKC resulting in steroid induced glaucoma in paediatric age group." IP Int J Ocul Oncol Oculoplasty 7, no. 1 (2021): 60-63. https://doi.org/10.18231/j.ijooo.2021.012
