- Visibility 116 Views
- Downloads 19 Downloads
- DOI 10.18231/j.ijooo.2021.005
-
CrossMark
- Citation
Orbicularis Bi-Pedicle flap: A single-staged surgical technique for the reconstruction of large and shallow, upper or lower eyelid defect
Introduction
An eyelid defect may present to an oculoplastic surgeon following trauma, tumour excision, irradiation or as a congenital coloboma. Its reconstruction is indicated if it may lead to complications like corneal exposure, constant epiphora (due to ectropion lower lid), exposure keratopathy (an irritable, dry eye), lid notching, lid retraction and lagophthalmos.[1] It is quite a challenging task, as the final outcome has to be almost perfect in order to restore the normal functional anatomy and aesthetics.
For the proper management of an eyelid defect, a thorough knowledge of the surgical anatomy of eyelids is mandatory.[2] The eyelids are made up of two lamellae, the anterior and a posterior. The anterior lamella comprises of a thin, relaxed skin, without any subcutaneous tissue so as to permit a full excursion of eyelids during blinking. Scars can easily be hidden in incisions made parallel to or within the skin creases (the skin tension lines), which are present at right angles to the direction of action of the underlying muscle. The upper lid crease is an important landmark; its symmetry with the opposite upper lid should be kept in mind during an upper lid reconstruction.
The underlying protractor muscle, the orbicularis oculi, runs circularly around the bony orbit; its different parts perform important functions like involuntary blinking that is essential for spreading the tear film uniformly over the cornea (pre-septal part), forced blinking (orbital part), maintaining eyelids in close approximation to the globe (pre-tarsal part), whilst the Horner’s muscle (a narrow strip of pre-tarsal orbicularis) forms an important constituent of the lacrimal pump mechanism that helps in the drainage of lacrimal fluid.
The posterior lamella is made up of a firm connective tissue framework, the tarsal plate, which maintains the shape of the eyelids, stabilises the lid margins, and keeps them tightly approximated to the globe. It contains the meibomian glands that secrete meibum which is essential in maintaining the stability of tear film in between blinks. On the inside, the tarsal plate is lined with a mucous membrane, the conjunctiva, that loosely attaches the eyelids to the globe and allows them to move independent of each other and makes the excursion of eyelids over the globe smooth and frictionless. Any eyelid reconstructive procedure must comprise of all these four structures to ensure the complete structural and functional integrity of the eyelids.
Factors that should be considered regarding the best surgical option pre-operatively are:[3], [4]
Patient's age
In younger age group, the skin and muscles are tight; the tissues relax with increasing age. Hence, for young patients, a small defect is considered to be involving 25-35% of the lid length, a medium defect involves 35-45%, and a large defect involves greater than 55% of the lid length. For older patients with lax lids, a small defect is 35-45%, a medium is 45-55% and a large defect involves more than 65% of the lid length.
The size and orientation of the defect
While planning reconstruction of the eyelid, the surgeon must analyse the missing lamellar components, whether the defect extends to the canthi and assess the integrity of the lacrimal drainage apparatus. If the eyelid margin is spared, closure by local flap or a free skin graft may suffice. But if the lid margin is involved, surgical repair must restore its integrity to avoid subsequent lid notching. A small eyelid defect can easily be closed directly in most cases. It can be combined with cantholysis[5] to close a defect occupying up to 50% or more of the eyelid but excessive tension on the suture line must be avoided to prevent wound dehiscence and ptosis postoperatively, especially in the elderly.
Vascular supply to the surrounding tissues
This determines the site from where flaps or free grafts can be taken. The arterial anatomy of the eyelids and the importance to eyelid reconstruction has been described by Erdogmus and Gosva.[6] An important aspect of eyelid reconstruction is that a free graft requires blood supply from its bed in order to survive; one free graft cannot be placed over another free graft as both will be devoid of a blood supply.
Previous treatment receiveved e.g.
Surgical repair or irradiation; following irradiation, the local blood supply is compromised.
Age of the wound
In a recent injury, tissues are edematous and swollen. A primary repair must be done within 24 hours prior to tissue swelling. In older defects, tissue fibroses and scarring results in loss of skin and muscle elasticity.
Numerous surgical options for eyelid reconstruction have been around for a very long time. They are generally classified using the “reconstructive ladder” in terms of morbidity, proceeding from the least invasive to the most invasive. At the bottom of the ladder is secondary intention healing in which defects granulate over a period of weeks in a moist, semi-occlusive environment.[7]
Newer techniques are continually being introduced which undergo further refinements and modifications to make them as simple and complication-free as possible. However, the method of choice ultimately depends upon a combination of all the above mentioned factors.
The options available for reconstruction of small to medium sized lid defect are a direct closure which can be combined with lateral cantholysis or a Tenzel Rotational Flap.[8] The general principle of reconstruction is that one lamella can be constructed as a flap while the other can be replaced as a free graft or a flap, with an intact vascular supply. When planned and executed properly, local skin flaps allow for a rapid reconstruction with a reliable and adequate blood supply and a good skin colour/texture match.
For the reconstruction of large, full-thickness eyelid defects (greater than 2/3 of the horizontal width of the lid), the two-staged, lid-sharing techniques are generally popular: the Mustarde lid switch flap[9] that can be used for both upper and lower lid defects, the Hughes Procedure[10] or its modification[11] for the lower lid reconstruction while the Cutler-Beard Flap[12] is mostly preferred for the upper lid defect. In these techniques, at the first stage, tissues are borrowed partially from one eyelid to reconstruct the other and the eye is kept occluded by the borrowed tissues for at least 6 weeks. At a second stage, once tissue healing has occurred, the lids are opened. The borrowing of tissues from a normal lid can result in structural damage to the donor site (scarring or disfigurement), as well as being two-staged procedures, they involve a long healing time with ocular morbidity.
We describe here a simple surgical technique to reconstruct full-thickness defects of either the upper or the lower eyelid, involving more than 2/3rd of the lid length. This study was conducted to see how successful we were in achieving the following four goals with this single-staged procedure:
To provide a full eyelid closure: to protect the globe and prevent exposure keratopathy
To preserve the pre corneal tear-film: at the end of each blink, the eyelids must close onto each other like a zipper, and be firmly opposed to the globe so that the upper lid can pick up the tear-film from the lower tear meniscus and spread it uniformly over the cornea.
To maintain an unobstructed visual field
To recreate an aesthetically appealing and an almost normal looking eye
Materials and Methods
A prospective, interventional study was conducted at two tertiary referral centres, over a period of eight years, from Jan 2011 – Dec 2018. A total of 17 consecutive cases were included. There were 4 primary cases (biopsy proven) with tumour along the lid margin and extending deep to the orbicularis oculi muscle; 9 recurrent cases with tumour recurrence at the site of excision (performed elsewhere), and 4 secondary cases, with a full thickness, shallow, lid defect with a loss of more than two-thirds of the lid tissue (following tumour excision elsewhere), referred for secondary reconstruction. There were 10 cases of basal cell carcinoma, 5 cases had a squamous cell carcinoma and 2 cases with a sebaceous gland carcinoma. The upper lid was affected in 6 cases while the lower lid in 11 cases. The median age of patients was 62 years (range 45 - 71 years), with 9 female and 8 male patients.
A thorough medical as well as a clinical history was taken regarding the duration of lid tumour, associated pain, itching, increase in size, bleeding or discharge from the tumour, treatment received in the past, any general medical illness and systemic medications. A history of tumour recurrence at the same site or elsewhere on the face or body was also inquired about.
In the pre-operative clinical assessment, the exact site of the defect (lateral, central or medial), its size, depth (whether fixed to the orbicular oculi or the bone), extent: whether it extended to the canthii or involved the lacrimal drainage system and the lamella of the eyelid tissue that needed to be replaced (in the secondary cases) was noted in clinical records. An assessment of lid laxity, the mobility of surrounding tissues (the forehead, cheek), presence of any scars, condition of the other eyelid, pre auricular or cervical lymph nodes, and a complete ophthalmic examination was performed to note any ocular surface disease (dry eyes, exposure keratopathy, meibomian gland dysfunction).
The patients and their attendants were fully explained the procedure and the need for regular follow-ups. In three cases, tumour extended medially involving the lower lacrimal punctum; these patients were informed that an excision of lower punctum and canaliculus would result in epiphora that would require a DCR with a Lester-Jones tube, at a later date, as a secondary procedure. An informed verbal consent was taken and mentioned in the clinical records. All patients who were taking oral blood thinner medications were instructed to stop them at least 10 days prior to the date of surgery (to control intra-operative bleeding as well as post-operative swelling). The surgery was performed by a single surgeon (SI) under local anaesthesia. The patients were instructed to have their morning anti-hypertensive medications with breakfast prior to coming for surgery.
The surgical technique
Anaesthetic eye drops (amethocaine 1%) were instilled into the eye prior to skin preparation. The eyelid was infiltrated with a warm, local anaesthetic mixture of 3cc bupivacaine + 2 cc Xylocaine and 0.1 cc of adrenaline 1:200,000; the point of needle was directed away from the tumour to prevent accidental tumour penetration and consequent seedling.
In primary cases, (requiring a tumour excision and a simultaneous eyelid reconstruction), the whole extent of tumour was marked under the microscope by a marking pen, along with a 5 mm area of presumed healthy eyelid tissue around it. The tumour was excised along with the 5 mm of the surrounding healthy lid tissue. The bleeding was controlled by adrenaline soaked swabs and a cautious use of cautery applied to the bleeding vessels. A 4/0 silk traction suture was passed through the lateral and medial wound edges to hold them straight and the exact extent of lid defect was measured.
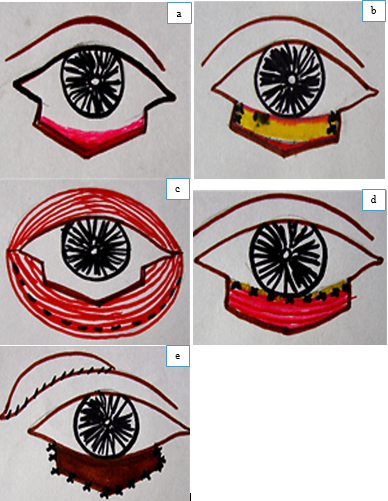
To reconstruct the posterior lamella first, after securing the haemostasis, the forniceal conjunctiva was ballooned by a sub-conjunctival injection of normal saline. Then it was mobilised from the lower fornix in case of a lower lid defect, and from the upper fornix in case of an upper lid defect ([Figure 1] a). Then a piece of donor sclera that was soaked in an antibiotic solution (gentamicin injection) for 2 hours, was trimmed according to the size of defect, and sutured to the remaining tarsus at the lateral and medial wound margins by a non-absorbable suture (ethibond 5/0) ([Table 2] b). In four cases, the wound extended to the lateral canthal angle, therefore the donor sclera was sutured either directly to the periosteum of the lateral orbital rim or its flap created to avoid tension on the suture line. In three cases, the tumour extended to the medial canthus, and the medial part of the lower lid had to be excised sacrificing the lower punctum and the canaliculus. The donor sclera was attached to the medial canthal tendon (MCT) in one case and to the anterior lacrimal crest in the other two cases where the MCT had to be excised due to a deep extension of the tumour.
Next, the mobilised conjunctiva was sutured to the upper border of donor sclera with a running 6/0 vicryl suture. Any tension in the conjunctival layer was relieved by a short, horizontal relaxing incision deep in the fornix. Then the lower lid retractors were identified and attached to the lower border of the scleral graft with a 6/0 vicryl suture. This step was important to prevent subsequent inward-bending of the posterior lamella and an entropion. In cases of the upper lid reconstruction, the levator aponeurosis was identified and sutured to the posterior margin of the donor sclera with a 6/0 vicryl suture.
In 2 cases of a shallow (horizontal width 3-5 mm), long, central upper eyelid defect, a partial thickness tarsal flap was dissected, everted and sutured into the defect over which the conjunctiva mobilised from the upper fornix was sutured.
To reconstruct the anterior lid lamella, the orbital or the remaining pre-septal portion of the orbicularis oculi muscle, that had retracted backwards into the orbit, was freed from the overlying skin and a 5 mm wide strip was split horizontally ([Figure 1]c) from the remaining muscle. This muscle strip remained attached by a medial and a lateral pedicle to the rest of the muscle at the canthal angles. The bi-pedicle flap, thus mobilised, was sutured to the upper border of the scleral graft with a 6/0 vicryl, continuous suture, taking bites of the mobilised conjunctiva as well ([Figure 1]d).
In cases with a central or a medial lid defect, a free graft of skin, 30% larger than the size of the defect, was taken either from the upper lid or the retro-auricular skin and sutured with a continuous 7/0 vicryl suture ([Figure 1]e). In four cases of a lateral lid defect, a Tenzel flap was used. Care was taken to keep the wound margins evenly approximated without tension and everted. Care was taken to keep the suture knots towards the skin side so as to avoid corneal irritation.
At the end of surgery, antibiotic ointment was instilled into the eye and the reconstructed eyelid was placed under traction for 5 days with a 4/0 silk traction suture to keep the lids closed, to stabilise the graft and to protect the eyeball. An antibiotic ointment was applied on the eyelids and covered by a pressure dressing for 72 hours. The wound was inspected and the dressing replaced for another 2 days. All cases were given oral antibiotic for 5 days, steroid/antibiotic skin cream for the reconstructed eyelid twice daily and a lubricating eye ointment at night.
Post-operative follow-up was after 1st and 2nd week and then after 1, 3, and finally at 6 months. At each visit, symptoms of disturbed vision, ocular discomfort, pain, irritation, watering or discharge from that eye was especially noted. On examination, visual acuity, status of the cornea, the pre-corneal tear-film and of the reconstructed lid was observed. Complications like lagophthalmos, ptosis, lid-retraction, entropion, ectropion, epiphora, corneal exposure or tumour recurrence were carefully looked for. Patient satisfaction was also noted in clinical records.


Results
The four parameters assessed both subjectively and objectively by a thorough clinical examination, as shown in [Table 2]. An unobstructed visual field was noted in all cases. Visual acuity was slightly reduced initially in the first post-operative week due to lid swelling and application of lubricant eye ointment in all cases. A full recovery occurred after one month.
Regarding the second parameter of affect on the pre corneal tearfilm, lagophthalmos was noted in 3 cases (27%) following upper lid reconstruction. This resulted in an incomplete blinking, tearfilm instability, a watery eye and punctate corneal staining noted in the 2nd week follow-up. This was managed by a downwards lid massage, lubricant eye drops during the day and ointment at night, with taping the lids together at night to avoid corneal exposure. The lagophthalmos gradually improved after 6 weeks.
A 2 mm lid retraction was noted in 2 cases (18%) following upper lid reconstruction. These two patients were a bit apprehensive regarding the aesthetic appearance. Since it persisted despite downwards lid massage for 3 months, it had to be managed surgically with a levator aponeurosis recession with hang-back sutures. An entropion of the upper lid margin was not noticed in any case. None of the cases of lower lid reconstruction had any complication like sagging of the lower lid, entropion or ectropion. All 17 patients (100%) were satisfied with the final cosmetic appearance at the 6 month follow-up. [Figure 2], [Figure 3] shows the pre-operative and post-operative results in two cases.
|
Characteristics |
Number |
% |
|
|
Gender |
Male |
8 |
47.06 |
|
|
Female |
9 |
52.94 |
|
Age |
Median |
62 years |
|
|
|
Range |
45 - 71 years |
|
|
Type of Presentation |
Primary tumor |
4 |
23.53 |
|
Recurrent tumor |
9 |
52.94 |
|
|
|
|
4 |
|
|
Histology of Tumour |
Basal Cell carcinoma |
10 |
58.82 |
|
|
Squamous cell carcinoma |
5 |
29.41 |
|
|
Sebaceous gland carcinoma |
2 |
11.76 |
|
Eyelid involved |
Upper lid |
6 |
35.29 |
|
|
Lower lid |
11 |
64.70 |
|
Location of eyelid defect |
Medial |
3 |
17.65 |
|
|
Central |
10 |
8.82 |
|
|
Lateral |
4 |
23.53 |
|
Parameters |
1st week |
1 month |
3 months |
6 months |
|
Visual Acuity |
Maintained: all 17 cases |
Reduced: 3 cases Maintained: 14 cases |
Maintained 17 cases |
Maintained 17 cases |
|
Ocular Discomfort |
3 cases |
3 cases |
nil |
nil |
|
Pain eye / lid |
nil |
nil |
nil |
nil |
|
Watery eye |
5 cases |
3 cases |
3 |
3 |
|
Discharge |
nil |
nil |
nil |
nil |
|
Tear maniscus |
formed |
formed |
formed |
formed |
|
Fluorescein staining cornea |
present: 3 cases |
present 3 cases |
nil |
nil |
|
Tearfilm BUT |
reduced 10 cases |
reduced 7 cases |
normal |
normal |
|
Blinking |
Incomplete 6 cases |
incomplete 5 cases |
incomplete 3 cases |
complete in all cases |
|
Lid Height/contour |
equal to opposite lid: all cases |
reduced upper lid height: 5 cases |
reduced lid height 2 cases |
restored equal to opposite lid all cases |
|
Patient satisfaction |
anxious |
Satisfied 15 cases Worried : 2 cases |
Satisfied 15 cases, Worried : 2 cases |
Satisfied All 100% |
|
|
|
|
|
|
|
Complications |
No of cases |
|
Entropion |
0 |
|
Ectropion |
0 |
|
Lag-ophthalmos & Punctate corneal staining |
3 (27%) |
|
Lid notching |
0 |
|
Lid sagging |
0 |
|
Lid retraction which needed levator recession |
2 (18%) |
|
No of dis-satisfied patients |
0 |
|
Total number of complications |
5 (45%) |
|
Total no of Satisfied Patients |
All 17 cases, 100% |
Discussion
Malignant eyelid tumours are quite common, comprising of 10% of all skin cancers.[13] Out of these, BCC is the commonest, as in our study too. Its frequent occurrence on the lower lid may be explained by the reflection of light from the cornea onto the lower lid margin or due to physical / chemical irritation by tears, whilst the upper lid is protected by the eyebrow.
A meticulous pre-operative assessment of the patient as a whole is very important, as was done in all our cases. The clinician must not only focus on the tumour but on the whole ocular surface and any ocular surface disease noted must be treated pre-operatively as it may get worse following surgery. We stopped the blood thinner medications (especially low-dose aspirin) pre-operatively to minimise intra-op bleeding and post-operative tissue swelling. This greatly reduces the post-operative recovery time.
The two surgical procedures widely recommended and preferred for skin cancers are the Mohs Micrographic Surgery (MMS)[14], [15] or a wide surgical excision with margin control and frozen section. MMS offers the maximal preservation of delicate eyelid tissue, prevents recurrence with a higher cure rate, and is cost effective because a secondary procedure is avoided.
For our patients, the facility for MMS or a simultaneous frozen section were not available. To achieve “margin control”, prevent/minimise micro-metastasis, and avoid tumour recurrence, the best available option was a wider resection of 5 mm healthy tissue surrounding the tumour with a full thickness lid resection.
After excising the tumour, traction sutures were applied at the lateral and medial margins of the defect to assess the exact dimensions that had to be reconstructed. We took particular care to minimise bleeding during surgery by stopping blood thinning medications preoperatively for 10 days, securing homeostasis by adrenaline-soaked swabs, a careful application of cautery to only large bleeding vessels, and applying a pressure dressing postoperatively. Excessive use of cautery was avoided to minimise tissue scarring post-operatively.
In reconstructing a full thickness lid defect, replacing the conjunctival lining is mandatory to permit a smooth excursion of the eyelid over the globe. The conjunctival fornices (both upper and lower) comprise of folds of loose, flexible conjunctiva that can be easily ballooned by a sub-conjunctival injection of saline. Therefore, it was easily mobilised and used to line the inner surface of the donor sclera in our cases; it also provided a vascularised bed for the overlying donor scleral graft. Any downward traction on the mobilised conjunctiva was avoided by a horizontal, relaxing incision deep in the fornix.
We used donor sclera to replace the tarsus in 15(88.2%) out of the total 17 cases, firstly, because it was readily available at our tertiary care facility (from donor eyes used for corneal grafts) and secondly, it reduced the surgical time that may be needed to obtain its alternatives like a rotational tarso-conjunctival graft, a hard palate or a nasal septal chondro-mucosal graft. Donor scleral graft provided a rigid support to the reconstructed lid margin; both its medial and the lateral margins were firmly anchored by a non-absorbable suture (5/0 ethibond) to the remaining tarsus or the periosteum of the orbital rim. Ethibond was preferred instead of Prolene as it was found to be relatively more pliable, the knots do not slip and the cut ends were not sharp. In only 2 cases (11.7%) with a shallow, central upper eyelid defect, a partial thickness tarsal flap was dissected, everted and sutured into the defect.
We attached the lower lid retractors to the lower border of the donor scleral strip to prevent both the outward movement of the reconstructed lower lid margin, as well as the inward bending of the upper lid margin, thus preventing an entropion. Similarly, while reconstructing the upper lid defect, a wider scleral graft was taken and the levator aponeurosis was approximated to it so as to avoid post-operative ptosis of the upper lid. The anchoring of levator muscle prevented the tendency of the overlying bi-pedicle flap to curl upon itself, preventing an entropion of upper lid and allowing the formation of a natural lid crease. Even though care was taken to avoid tightening of the levator aponeurosis and tissue scarring by a careful dissection, still lagophthalmos occurred in 3 cases while upper lid retraction of 2 mm in 2 cases (18%), that required levator muscle recession as a secondary procedure.
The presence of a free tissue graft in the posterior lamella (free tarsus, donor sclera, nasal septal chondro-mucosa or hard palate) necessitates an overlying vascularised flap to reconstruct the anterior lamella. In our cases, this was provided by mobilising a bi-pedicle flap of the orbicularis oculi muscle. The bi-pedicle muscle flap also retained its normal nerve supply, with the added advantage of maintaining muscle tone and the very crucial blink mechanism. The muscle tone kept the reconstructed eyelid in close approximation to the globe and stabilised the lid margin. In addition, the levator muscle attached to the upper lid scleral graft and lower lid retractors inserted into the lower scleral graft, combined with an intact innervation of the orbicularis flap, maintained the natural mobility of the reconstructed eyelid.
The eyelid skin is naturally very thin and flexible. In cases where the patient had an excessive, lax upper lid skin, a free graft was taken either from the same eye or the opposite eye to ensure a perfect match of colour and texture. In cases where no extra eyelid skin was available a free skin graft was taken from the retro-auricular region or a semi-circular skin flap (Tenzel) for a lateral lid defect.
The use of an orbicularis myocutaneous flap was initially described by Moschella et al in 1995.[16] They used orbicularis bipedicle myocutaneous flap from the preseptal orbicularis to reconstruct large, full thickness upper eyelid defects in only 2 cases. This was lined by a free buccal mucosal graft, on its under side, and the donor site was covered by transpositioning a tempo-frontal flap. They felt that replacing the tarsus was not necessary, and the absence of a cartilaginous layer allowed a better adherence of muscle flap with the mucosal graft. Their one case (50%) developed entropion post-operatively. Since none of our cases developed an entropion or an ectropion shows that the presence of a rigid eyelid support is mandatory in reconstructing a full-thickness defect. The donor scleral graft used in our cases resulted in a better longterm stability and mobility of both the upper and lower lids.
We feel that an Orbicularis myocutaneous flap is sufficient only to replace a large anterior lamellar defect. Han et al[17] used the myocutaneous orbicular island flap to reconstruct superficial, medial and lateral canthal defects in 7 cases with good results. This flap has also been used in upper lid blepharoplasty. Lower eyelid is a direct continuation of the cheek tissues, hence defects involving the entire lower eyelid may be reconstructed using a Mustarde cheek rotation flap.[18] This flap comprises of skin, subcutaneous tissue and the orbicularis which is adequate for a lid defect involving only the anterior lamella. But for a full-thickness defect, without the support provided by the tarsal plate, lower lid ectropion can result from anterior lamella shortening or lower lid laxity, worsened by the affect of gravity resulting in an altered lid mobility.
This fact has been taken into account in other studies too. Demir et al[19] described the reconstruction of a large upper lid defect by a V shaped orbicularis oculi myocutaneous flap, advanced from the remaining eyelid tissue to reconstruct the anterior lamella; the posterior lamella was reconstructed with a mucoperiosteal graft harvested from the hard palate. Matsuo et al[20] reconstructed a mid-lateral lid margin defect by an orbicularis oculi musculo-cutaneous advancement flap for the anterior lamella, combined with a free conchal cartilage graft for the posterior lamellar reconstruction. The authors found this technique to be simple, less invasive and single staged.
The reconstruction of upper eyelid is a lot more challenging than the lower one as it has to perform numerous important functions as well as matching the other eye aesthetically. All these factors were kept in mind during the reconstructive procedures of all cases in our study.
Conclusion
The surgical technique we described in this study is a simple, single-staged procedure with a short learning curve. It did not cause any damage to the other eyelid and was associated with a minimal number of complications that were easily managed. It was less invasive than the two-staged, lid-sharing procedures and resulted in a functional, dynamic, and an aesthetic reconstruction. It is particularly recommended in monocular patients and in children who are predisposed to occlusion amblyopia.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- M A Codner, A B Weinfeld. Pr47 comprehensive eyelid reconstruction. ANZ J Surg 2007. [Google Scholar] [Crossref]
- B Patel, A D Meyers. Eyelid anatomy. 2013. [Google Scholar]
- Mounir Bashour, L M Vistnes. Lower Eyelid Reconstruction. 2013. [Google Scholar]
- IM Mathijssen, JC van der Meulen. Guidelines for reconstruction of the eyelids and canthal regions. J Plast Reconstr Aesthet Surg 2010. [Google Scholar] [Crossref]
- JB Holds, RL Anderson. Medial Canthotomy and Cantholysis in Eyelid Reconstruction. Am J Ophthalmol 1993. [Google Scholar]
- S Erdogmus, F Govsa. The arterial anatomy of the eyelid: importance for reconstructive and aesthetic surgery. J Plast Reconstr Aesthet Surg 2007. [Google Scholar] [Crossref]
- JC Lowry, GB Bartley, JA Garrity. The Role of Second-Intention Healing in Periocular Reconstruction. Ophthal Plast Reconstr Surg 1997. [Google Scholar] [Crossref]
- J R Boynton. Semicircle flap reconstruction "plus. Ophthalmic Surg 1993. [Google Scholar]
- J Ambrozová, J Mesták, J Smutková. Reconstruction of the lower eyelid after excision of major tumours. Acta Chir Plast 1993. [Google Scholar]
- P L Custer. Tarsal kinking after Hughes flap. Ophthal Plast Reconstr Surg 1998. [Google Scholar] [Crossref]
- RJ Rohrich, RIS Zbar. The Evolution of the Hughes Tarsoconjunctival Flap for Lower Eyelid Reconstruction. Plast Reconstr Surg 1999. [Google Scholar] [Crossref]
- N L Cutler, C Beard. A Method for Partial and Total Upper Lid Reconstruction. Am J Ophthalmol 1955. [Google Scholar] [Crossref]
- A Echchaoui, M Benyachou, A Houssa, M Kajout, A A Oufkir, C Hajji. Management of eyelid carcinomas. J Fr Ophtalmol 2016. [Google Scholar]
- D T Harvey, S R Taylor, K M Itani, R J Loewinger. Mohs Micrographic Surgery of the Eyelid: An Overview of Anatomy, Pathophysiology, and Reconstruction Options. Dermatol Surg 2013. [Google Scholar] [Crossref]
- R Malhotra, S C Huilgol, N T Huynh, D Selva. The Australian Mohs database, part I: periocular basal cell carcinoma experience over 7 years. Ophthalmol 2004. [Google Scholar]
- F Moschella, A Cordova. Upper eyelid reconstruction with mucosa-lined bipedicled myocutaneous flaps. Br J Plast Surg 1995. [Google Scholar] [Crossref]
- J Han, S T Kwon, S W Kim, E C Jeong. Medial and lateral canthal reconstruction with an orbicularis oculi myocutaneous island flap. Arch Plast Surg 2015. [Google Scholar]
- M A Callahan, A Callahan. Mustardé Flap Lower Lid Reconstruction after Malignancy. Ophthalmol 1980. [Google Scholar] [Crossref]
- Z Demir, S Yuce, S Karamursel, S Celebioglu. Orbicularis oculi myocutaneous advancement flap for upper eyelid reconstruction. Plast Reconstr Surg 2008. [Google Scholar]
- K Matsuo, Y Sakaguchi, M Kiyono, Y Hatana, T Hirose. Lid Margin Reconstruction with an Orbicularis Oculi Musculocutaneous Advancement Flap and a Conchal Cartilage Graft. Plast Reconstr Surg 1991. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Irfan S. Orbicularis Bi-Pedicle flap: A single-staged surgical technique for the reconstruction of large and shallow, upper or lower eyelid defect [Internet]. IP Int J Ocul Oncol Oculoplasty. 2025 [cited 2025 Sep 04];7(1):17-24. Available from: https://doi.org/10.18231/j.ijooo.2021.005
APA
Irfan, S. (2025). Orbicularis Bi-Pedicle flap: A single-staged surgical technique for the reconstruction of large and shallow, upper or lower eyelid defect. IP Int J Ocul Oncol Oculoplasty, 7(1), 17-24. https://doi.org/10.18231/j.ijooo.2021.005
MLA
Irfan, Sameera. "Orbicularis Bi-Pedicle flap: A single-staged surgical technique for the reconstruction of large and shallow, upper or lower eyelid defect." IP Int J Ocul Oncol Oculoplasty, vol. 7, no. 1, 2025, pp. 17-24. https://doi.org/10.18231/j.ijooo.2021.005
Chicago
Irfan, S.. "Orbicularis Bi-Pedicle flap: A single-staged surgical technique for the reconstruction of large and shallow, upper or lower eyelid defect." IP Int J Ocul Oncol Oculoplasty 7, no. 1 (2025): 17-24. https://doi.org/10.18231/j.ijooo.2021.005
