- Visibility 80 Views
- Downloads 9 Downloads
- DOI 10.18231/j.ijooo.2021.003
-
CrossMark
- Citation
Surgical approaches to the orbit - The past and the present
- Author Details:
-
Deepsekhar Das
-
Sujeeth Modaboyina
-
Saloni Gupta
-
Aarush Deora
-
Sahil Agrawal *
Introduction
The knowledge regarding human anatomy and physiology have progressed with leaps and bounds in the last two centuries. The diseases of the orbit which were once thought to be not curable can be treated with ease in the present day. Recent advances in instrumentation and techniques of orbitotomy have given optimal access to orbital lesions with minimal or no functional injury and good esthetic outcomes.
In the current scenario, an ophthalmic surgeon practicing oncology should have a piece of adequate knowledge regarding all possible treatment modalities available for any pathological lesion to manage the disease successfully. When surgery of the orbit is being considered, it is essential to plan what type of approach can be used to the best advantage and the surgical goal (biopsy/ excision/ debulking).
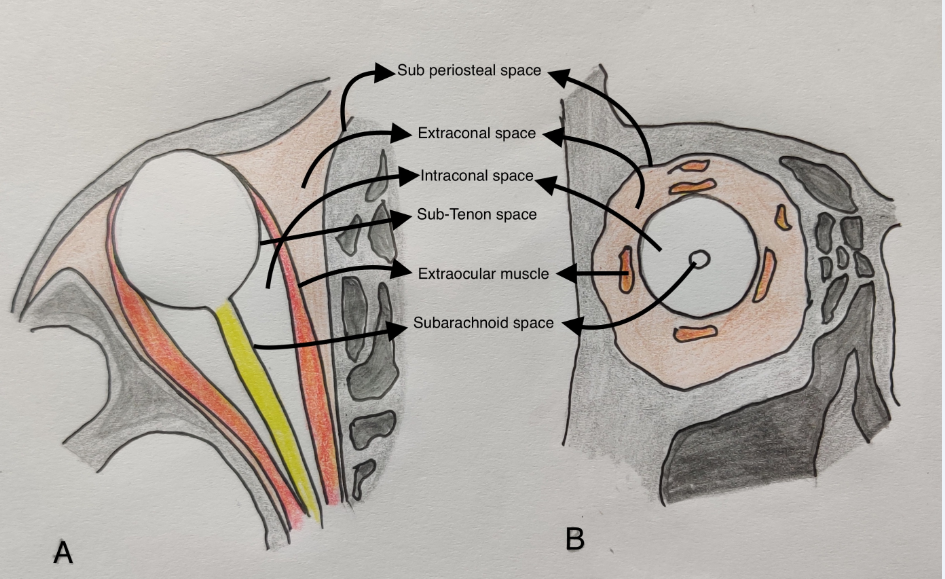
A good experience in the surgical anatomy of orbit and its related spaces is essential for planning the type of approach. Orbit is a pyramidal shape structure that can be approached by transcutaneous or transconjunctival route in the superior, inferior, lateral and medial approach. There are five surgical spaces in orbit ([Figure 1]): subperiosteal (between the bone and the periorbital), extraconal surgical space (periorbita and the muscle cone with its fascia, sub-tenon surgical space (between the tenon capsule and the globe), intraconal surgical space (within the muscle cone) and subarachnoid surgical space (between the optic nerve and the nerve sheath). A single orbital lesion may involve more than 1 surgical space, and a combination of approaches may be necessary for pathologic lesions affecting the orbit.
There is no definite nomenclature or classification of orbitotomy approaches. It is broadly divided into anterior orbitotomy and lateral orbitotomy. Anterior orbitotomy in general means that the approach is usually through the eyelid or conjunctiva from the front of the orbit. Anterior routes include the superior, inferior, medial, and transconjunctival approaches. Lateral orbitotomy in general, means that the approach is from the lateral side of the orbit wherein the lateral rim will be removed. The transcranial route is best suited for orbital apex.

Evolution of orbitotomy approaches
In the golden era of the ‘Greeks’ and ‘Romans’; proptosis was managed by performing venesection and purging on patients.[1] In the 10th century, Ali Ibn Isa treated proptosis by immersing face in cold saline water; upon failure of response lead plate was adjusted over the eye and it was left at gods mercy.
Extirpation or the present-day subtotal exenteration was performed by Bartisch in the late 1500s period for the outward protruding eyeball. The procedure involved impaling the eyeball with strong needle and thread for manipulation and traction. He then used spoon-shaped knife for extirpation of ocular tissues till bone has be reached leaving behind eyelids intact. One can read and only imagine how dreadful and inhumane this procedure was before the advent of anesthesia.
Orbital tumor removal through lower lid trans cutaneous route was first described by Thomas Hope of Scotland in a young girl with preservation of the globe.[2] Hope credited his mentor, the famous French ophthalmologist, St. Yves, as having first successfully performed such an operation. Parker described using a transconjunctival incision in order to remove a cystic lesion from the lateral orbit most likely dermoid.[3] De wecker and Carter also used lateral transconjunctival approach for accessing optic nerve.[4] The difference in their approaches was that De wecker approached optic nerve by splitting tenons between lateral and inferior rectus followed by globe prolapse, whereas Carter disinserted lateral rectus which gave good visualization of optic nerve which was absent in De weckers technique. Herman Knapp also used a transconjunctival route for a tumor located in the deep intraconal space surrounding the optic nerve which was successfully removed with preservation of globe though vision could not be preserved.[5]
Passavant was the first surgeon to perform lateral orbitotomy for an orbital vascular malformation. Independently Kronlein popular method of lateral orbitotomy performed by creating a crescent-shaped skin incision in the lateral side of orbit with the anterior convexity at the lateral orbital rim, and extending superiorly towards the hairline and inferiorly towards the ear.[6] In his procedure creation of bone window increased access to the deep orbital tumors. The limitation of this procedure were limited working space and ugly postoperative scar.[7] In 1901 Cirincione performed lateral orbitotomy by using S-shaped incision starting under brow.[8]
In 1907, Rollet reported the first anterior orbitotomy, which involved making an incision beneath the brow and dissecting subperiosteally in order to gain entry to the orbit.[9] Fronto ethmoidal mucocele with proptosis was managed by Lynch by placing incision in the superomedial orbital rim which extended from supratrochlear region to medial canthal area.[10] This incision however, had complications like globe luxation into nasal cavity, webbing of medial canthal area, lacrimal system injury and superior oblique tendon injury.
Roentgen was the only imaging modality available at that time it was difficult to identify the intracranial extension. The limitation of incomplete removal of tumors with intracranial extension was overcome by Walter Dandy in 1922 by his intracranial approach.[11] However, Dandy advocated exclusively transcranial approach for orbital tumors, though the most common cause of proptosis was endocrine related. Moreover, transcranial approach had limitations like mortality (4%), incomplete removal of tumor, meningitis, rhinorrhea, superior rectus weakness and ptosis. Davis approached optic nerve tumors by using lower lid incision.[12] Reese performed lateral orbitotomy by direct incision on lateral canthus followed by canthotomy for approaching lesions located in deep orbit.[13] Benedict introduced brow incision followed by periosteal elevation for nasal or temporal located superficial tumors.[14] He also advocated transcranial approach for deep orbital tumors not accessible by his approach.
From 1886 to 1940, the majority of eye surgeons regarded the orbit as a deep, dark and bloody field with unrewarding surgical results. In 1947 Stallard performed lateral orbitotomy by using the Kroleins method but instead of crescent incision he used S shaped incision which was earlier described by Cirincione.[15] The incision started in the lower end of lateral sub brow region, followed the curve of zygomatic arch and in the center of the arch, horizontal incision is placed. Similar incision was described by Dickson Wright which was later came to be known as classic Stellard-Wright incision. This incision had a complication of injury to facial nerve branches. Later it was modified into more curvilinear manner with shortened horizontal limb. The supra orbital part of the incision is hidden under eyebrow and the horizontal part under the skin fold of crow’s feet making the incision cosmetically acceptable.
Raynold Berke’s modified Kronleins approach by increasing the size of bony window from triangle to rectangle shape.[7] In 1962, Byron Smith described lid splitting incision to gain access to the anterior superomedial orbit.[16] Leone and Wolfley described the use of an incision in the natural upper eyelid crease to obtain access to the superomedial orbit.[17], [18] The advantages of such an approach include a familiar route to the eyelid and the anterior orbit, minimal dissection with little risk to vital structures, excellent exposure of orbital structures, and simple wound closure with a practically unnoticeable scar.
Jones in 1970 first described trans-frontal approach for tumors located superior to optic nerve in mid to posterior orbit.[19] Later in 1982, Jane described a supraorbital approach to tumors and aneurysms of the suprasellar area, as well as to orbital lesions.[20] Al-Mefty modified this approach by incorporating the superior and lateral orbital walls.[21] Delashaw described the temporal and orbital extension of the supraorbital exposure.[22] The inferior extension of the supraorbital craniotomy by removal of the orbital rim was also described by Delfini using an alternative technique with two bone flaps.[23] Rootman rightly described these procedures as “Panoramic Orbitotomy” owing to wide field of exposure for surgeons.[24]
A cosmetically acceptable incision in place of lynch incision was given by Balch in 1998 in the form of transcaruncular approach, which gave access to deep part of medial orbit upto apex.[25] Garcia also described similar approach but for treating medial wall fracture or orbit.[26] Later this incision was popularized by Goldberg.[27] In 1999 Herman described trans-nasal endoscopic approach in a case of inferomedial located orbital cavernous hemangioma in the posterior orbit.[28]
|
Extraconal lesions |
Intraconal Lesions |
Medial Orbital Lesions |
|
Frameless image-guided neuronavigation |
Transconjunctival endoscopic approach. |
Frameless image-guided neuronavigation. |
|
Finger’s aspiration cutter technique for superficial lesions |
Finger’s aspiration cutter technique for biopsies |
Trans-caruncular for front-ethmoidal mucoceles. |
|
Lateral triangle flap for endoscopic approach |
|
|
Recent advances
In 2002 Lai et al. conducted a study where they used a trans-caruncular approach in order to remove frontoethmoidal mucoceles. The authors made an incision over the caruncle to reach the medial orbital wall periosteum and obtained a good exposure of the mucocele and removed them. They used to put a trans-nasal tube before closing the wound. It was concluded that transcaruncular approach was safe and provided a wide exposure for medial orbital.[29]
In 2005 Nemet et al. described a “Lateral triangle flap” technique, where the authors made an upper eyelid skin crease incision and skin incision from the lateral canthal angle. The incisions were joined laterally at the outer margin of the lateral orbital rim, just beyond the lateral orbital margin. The triangular skin muscle flap was raised medially, based at the canthal angle, providing maximal exposure of the lateral and superolateral orbital wall. The method was found to provide good exposure and satisfactory cosmetic outcomes.[30]
A lateral retrocanthal, minimally invasive, canthus sparing approach was published by Moe et al in 2007. The authors initially conducted a cadaver study to develop a transconjunctival lateral surgical technique in order to reach the orbital floor and roof without effecting the structural integrity of the eyelid support system. They performed the technique on 30 patients and eventually found this procedure to be safe yet providing a rapid access to the lateral orbit with ample exposure. They also added that this incision could be extended in a single continuous incision to the medial orbit. However, the structural integrity of the lateral retinaculum was unaffected. The wound healing was rapid, without tissue distortion or scars.[31]
Pillai et al. in 2008 described the transconjunctival endoscopic approach to the optic nerve and the medial intraconal orbit using a 2.7 mm diameter rigid endoscope in 7 cadavers. He concluded that the procedure is easy to perform and does not cause much damage to the adjacent muscles. Infact, it can result in cosmetically satisfying outcomes.[32]
Finger et al. in 2011 published a new technique of obtaining an orbital biopsy using the vitrectomy cutter. In this technique also known as “Finger’s aspiration cutter technique(FACT)’’, first the lesion is palpated, and entry sites are marked with stains. Based on the site, an incision is made using either a Wescott scissors for conjunctiva or a no 11 blade for skin; the vitrectomy cutter shafts were entered and using a bimanual technique; holding the lesion by one hand and controlling the vitrectomy cutter with the other, biopsy was obtained. The advantage of this procedure was that it does not require any sutures.[33]
The endoscopic approach to the lateral orbit was employed by Lyson et al. in 2014, where he initially used navigation guided target marking, followed by a 1.5cm skin incision within a skin wrinkle behind the lateral canthus. Using a bone drill an opening was created in the lateral orbital wall to gain access to the orbital compartment. They were able to successfully remove extraconal epitheliod hemangiomas and extraconal cavernous angiomas in the lateral retrobulbar space.[34]
Similarly, GuangMing Zhou in November 2018 described the use of navigation-guided endoscopy combined with deep lateral orbitotomy for removing small tumors at the lateral orbital apex. After skin incision, exposure of the lateral wall and its fracture, a navigation-guided microdrill and rongeur were used to remove the greater wing of the sphenoid bone posteriorly until the dura mater was encountered to provide adequate exposure of the orbital apex. After this, intraorbital dissection was performed with a standard endoscope guided by navigation, tumor was visualized and thus removed. It seemed to be a feasible, efficient, and safe approach.[35]
In 21st century, there has been a boom in the incorporation of various imaging modalities in the planning of orbital surgeries. The first description of “Frameless image-guided neuronavigation” in orbital surgery was published by Hejazi et al. in 2005. The author used a frameless infrared-based neuronavigation system in the microsurgical removal of 11 orbital tumors. He used a transconjunctival approach in the removal of the tumours. The study concluded that the use of the navigation system reduces the intra-operative risk and increased the effectiveness of microsurgical orbital procedures.[35]
Surgical approaches
Anterior approach
The majority of the anterior orbitotomy techniques are used for biopsy of masses palpable through the skin or the conjunctival fornices mainly in the extraconal space. Anterior orbitotomy include the superior, inferior, medial, and transconjunctival approaches.
Superior approach
This is excellent for superior extraconal lesions of the orbit including the lacrimal gland tumors. Superiorly there are two basic approaches, the lid crease and the sub-brow incision. The upper eyelid skin crease incision (modified Stallard-Wright incision) starts from the puncta to the lateral canthus and then extends laterally along the laugh line without damaging the lateral canthus to reach upto the zygomatic arch. Dissection is carried out through the orbicularis muscle to reach the septum. The mass can now be easily palpable, the septum is cut open to perform the biopsy (excisional/incisional) and skin closure is done. The sub brow incision is curvilinear and parallel to the arch of the superior orbital rim and slightly below it. The length of the incision can be varied according to position of the mass, keeping the area where the palpable mass lies as midpoint of the incision and can be extended nasally or medially to accommodate the necessary surgical exposure.
Inferior approach
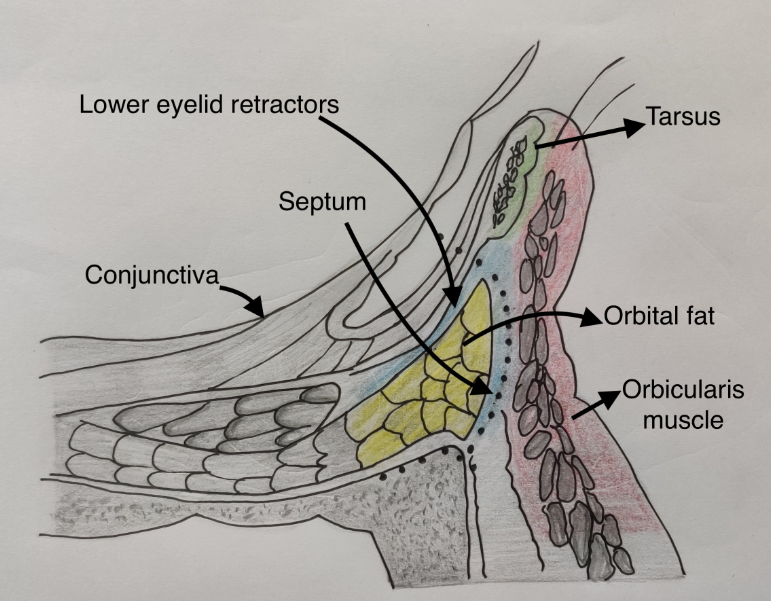
The masses palpable in the inferior extraconal space can be approached through the lower eyelid transcutaneous incision (sub ciliary or infraorbital), or a transconjunctival approach. In transcutaneous approach an incision is marked 2mm below the lash line from puncta to lateral canthus, dissection post which is carried out similar to the superior approach.
For transconjunctival inferior approach, after a conjunctival incision is made 3 mm inferior to the tarsal border, dissection is carried through the insertion of the lower lid retractors, and then inferiorly in an avascular plane toward the orbital rim. The dissection can proceed in either a preseptal or postseptal plane. The preseptal approach (preferred) avoids the orbital fat manipulation thereby helps in better visualization as caused by obscuration of the surgical view from prolapsed orbital fat. Conversely, the postseptal plane provides a more direct approach to the orbital fat pads, and is particularly useful in lower eyelid blepharoplasty.[36] Once the dissection has reached the level of the orbital rim, careful elevation of the periosteum provides easy access to the subperiosteal space along the orbital floor or the face of the zygoma.
When more exposure of the lateral rim is needed, including access to the frontozygomatic suture, the incision is lengthened; after a canthotomy, skin incision in made at lateral canthus, inferior cantholysis is achieved and the transconjunctival incision is then made as previously described.
When access to the medial orbit is necessary, the transconjunctival incision can be combined with a transcaruncular incision.[37], [38] This modification is called as Mc Cord lid swinging incision. This combination along with elevating the inferior oblique muscle from its attachment at the inferior orbital rim allows wide access to the orbital floor and medial wall.
Medial approach
This approach is best suited for accessing the sub-tenons and medial intraconal superficial and deep spaces of the orbit. It comprises of the transcutaneous fronto-ethmoid, transcutaneous/trans marginal lid split, transcaruncular, transconjunctival and transnasal endoscopic approach to access the apex.
For a transconjunctival medial orbitotomy, 180o medial conjunctival peritomy is done, with radial relaxing incisions on the bulbar conjunctiva to improvise the exposure. Sub tenons careful dissection opens up the intraconal space and a disinsertion of the medial rectus can aid in accessing deeper orbit.
The vertical lid splitting incision is used for deeper areas of the extraconal and intraconal space of the medial orbit. A vertical lid split is done at a line situated at medial one third of the eyelid. The incision extends above the tarsus and is carried deep to split the eyelid dividing the levator aponeurosis-mullers-conjunctival complex as a whole. This method has difficulty in accessing the posterior one third of the medial intraconal space. Transcutaneous fronto-ethmoid or the Lynch incision is placed as an arch midway between the bridge of the nose and the medial canthus, extending form the inferior to the superior orbital rim following the natural concavity of the medial canthus. The dissection is carried deep, the periosteum of the inferior and medial orbit is reflected and the lacrimal sac elevated. It is helpful for accessing the medial extraconal and subperiosteal spaces when other routes don’t give adequate exposure as it leaves behind a ugly scar because of the webbing across the medial canthus.
The transcaruncular approach helps in reaching the extraconal and subperiosteal medial orbital spaces, used mainly for repairing a medial wall fracture and for orbital decompression as a part of ethmoidectomy. Using Westcott scissors, area between the plica semilunaris and the caruncle is cut open and bluntly dissected down to reach the periosteum, taking care of the ethmoidal vessels.
Lateral orbitotomy
Lateral orbitotomy with bone cutting provides enormous space to access both the extra and intra conal spaces of the lateral orbit. It involves a horizontal skin incision starting from the lateral canthal angle extending laterally for about 10mm and dissecting subcutaneously to reach the lateral orbital rim. The periosteum is then incised 2mm posterior to the lateral orbital rim and elevated posteriorly toward the temporal fascia. The temporalis fascia is cut open about 1-2 cm to allow access to temporal fossa, wherein the temporalis muscle is elevated at the posterior edge of the lateral orbital rim. For removing the bone, the superior cut is made at or above the frontozygomatic suture and the inferior one at the junction of zygomatic arch to the lateral orbital rim using a power saw. Care is to be taken while cutting through the superior mark, by closely observing the area where the lateral wall becomes thickened to become the floor of the anterior cranial fossa. Before removing the bone as a whole, holes for repositioning the bone later are drilled, planking across the bony incisions. The bone is then out fractured using a rongeur. The periorbita is then opened in a T shaped fashion, with the longer limb of T running parallel to the lateral rectus. Once the biopsy is done, the bone may be replaced using screws and microplates, or sutures.
The lateral parts of the orbit, however, can also be readily reached through a horizontal lateral canthotomy without mobilizing bone or dividing the crura of the lateral canthal tendons. This innovative canthotomy approach gives access lateral to the optic nerve, both the intra and extraconal space, and allows easy tissue sampling of a diffuse intraorbital pathology from several diverse tissues.[39]
Transcranial approach
Though trancaruncular and the fronto ethmoid approach provides limited access to the orbital apex, for access to those dep medial orbital tumors situated in conjunction to the optic nerve, transcranial approach is best suited. There are three transcranial approaches namely, frontal transcranial/ panoramic orbitotomy, eyebrow craniotomy and pterioanl craniotomy. In fronto transcranial orbitotomy, superior orbital rim and anterior portion of the orbital roof are flapped open exposing the superior orbital periorbita. The eyebrow craniotomy gives acess to frontal lobe and the anterior orbit, by removing window of frontal bone, from a 3-4 cm long incision made above the eyebrow hairs. In pterional craniotomy approach, bone around the superior orbital fissure is removed with removing the optic strut and the anterior clinoid process. The lateral wall and roof of the optic canal can also be removed.
Image Guided Orbital Surgery
There are a number of different systems available, including InstaTrak (Visualization Technology Inc., Woburn, MA, USA), LandmarX (Xomed-Medtronic, Jacksonville, FL, USA), Cygnus PFS System (Compass International, Rochester, MN, USA), and Stealth Station (Medtronics, Memphis, TN, USA). Each carry their own advantages and disadvantages. The InstaTrak system involves a plastic headset (anchored at the external auditory canals bilaterally and the nasal dorsum) followed by the acquisition of a CT or magnetic resonance (MR) scan. At the time of surgery, a probe helps in transmitting the images through the plastic headset placed back on the patient. The Stealth system requires a preoperative MR scan, before which several adhesive fiducials on the scalp needs to be placed. At the time of surgery, a probe with a light-emitting diode registers the markers and allows for localization on the preoperative scan. The Cygnus PFS system differs from the Stealth as it uses magnetic special referencing and tracking, however, is similar in its use of fiducial markers yet. The LandmarX system requires preoperative CT, and instead of the need of the patient to wear a headset or have fiducial markers placed ,a 3-camera system located 6 feet from the head of the surgical table collects information from light-emitting diodes which are on a headset placed on the patient's head at the time of surgery. This allows for real-time positioning of surgical instruments using infrared tracking and thereby mobility of the head intraoperatively.[39], [40]
Conclusion
Most of the tumours can be approached from the front of the orbit through anterior orbitotomy while others located deep in the orbit may require advanced procedures. Understanding the surgical spaces of the orbit will help in an anatomic approach that will guide us to choose the procedure as well as helps in navigating the orbit itself.
Authors Contribution
Deepsekhar Das MD and Saloni Gupta MS, Both the authors have equal contribution for authorship
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- J W Henderson, G M Farrow. Orbital Tumors. 2013. [Google Scholar]
- T Hope. An account of’; remarkable cure performed on the eye of a young woman in Scotland. Phil Tram R Sot Land 1744. [Google Scholar]
- JA Khan, DM Albert. Willard Parker's 1841 orbital operation. Survey Ophthalmol 1988. [Google Scholar] [Crossref]
- F A Billson, R L Hudson. Surgical treatment of chronic papilloedema in children.. Br J Ophthalmol 1975. [Google Scholar] [Crossref]
- H Knapp. A case of carcinoma of the outer sheath of the optic nerve, removed with preservation of the eyeball. Arch Ophthalmol 1874. [Google Scholar]
- R U Kronlein. Zur Pathologic und operativen Berhandlung der Dermoidcysten der Orbita. Beitr Klin Chir 1988. [Google Scholar]
- R N Berke. A modified Krönlein operation. Trans Am Ophthalmol Soc 1953. [Google Scholar] [Crossref]
- H B Stallard. The evolution of lateral orbitotomy. Trans Ophthalmol Soc UK 1973. [Google Scholar]
- B Smith. The anterior surgical approach to orbital tumors. Trans Am Acad Ophthalmol Otolayngol 1966. [Google Scholar]
- V J Lund, M E Rolfe. Ophthalmic considerations in fronto-ethmoidal mucocoeles. J Laryngology Otol 1989. [Google Scholar] [Crossref]
- S Duke-Elder, P A Macfaul. The ccular adnexa. In: Duke-Elder S.System of ophthalmology, v13: pt 1 Diseases of the Eyelids; pt 2 Lacrimal, Orbital and Para-Orbital Diseases. 1974. [Google Scholar]
- Davis. Primary tumors of the optic nerve (a phenomenon of recklinghausen's disease): a clinical and pathologic study with a report of five cases and a review of the literature. Arch ophthalmol 1940. [Google Scholar]
- A Reese. Orbital Tumors and Their Surgical Treatment. Am J Ophth 1941. [Google Scholar]
- W L Benedict. Surgical treatment of tumors and cysts of the orbit: the eleventh de Schweinitz lecture. Am J Ophthalmol 1949. [Google Scholar]
- HB Stallard. A plea for lateral orbitotomy: with certain modifications. Br J Ophthalmol 1960. [Google Scholar] [Crossref]
- B Smith. The anterior surgical approach to orbital tumors. Trans Am Acad Ophthalmol Otolaryngol 1966. [Google Scholar]
- CR Leone. Surgical Approaches to the Orbit. Ophthalmol 1979. [Google Scholar] [Crossref]
- D E Wolfley. The lid crease approach to the superomedial orbit. Ophthalmic Surg 1985. [Google Scholar]
- B R Jones. Surgical approaches to the orbit. Trans Ophthalmol Soc UK 1970. [Google Scholar]
- J A Jane, T S Park, L H Pobereskin, H R Winn, A B Butler. The supraorbital approach: technical note. Neurosurgery 1982. [Google Scholar]
- O Al-Mefty, JL Fox. Superolateral orbital exposure and reconstruction. Surg Neurol 1985. [Google Scholar] [Crossref]
- JB Delashaw, JA Jane, NF Kassell, C Luce. Supraorbital craniotomy by fracture of the anterior orbital roof. J Neurosurg 1993. [Google Scholar] [Crossref]
- R Delfini, A Raco, M Aritco, M Salvati, P Ciappetta. A two-step supraorbital approach to lesions of the orbital apex. J Neurosurg 1992. [Google Scholar] [Crossref]
- J Rootman, B Stewart, R A Goldberg, Eds. Orbital Surgery: A Conceptual Approach. New York: Lippincott Williams & Wilkins 1995. [Google Scholar]
- K C Balch, R A Goldberg, J P Green. The transcaruncular approach to the medial orbit and ethmoid sinus. Facial Plast Surg Clin North Am 1998. [Google Scholar]
- G H Garcia, R A Goldberg, N Shorr. The transcaruncular approach in repair of orbital fractures: a retrospective study. J Cranio-Maxillofacial Trauma 1998. [Google Scholar]
- RA Goldberg, R Mancini, JL Demer. The Transcaruncular Approach. Arch Facial Plast Surg 2007. [Google Scholar] [Crossref]
- G Lot, F Portier, P Herman, B Silhouette, M Wassef, R Marianowski. Transnasal Endoscopic Removal of an Orbital Cavernoma. Ann Otol, Rhinol Laryngology 1999. [Google Scholar] [Crossref]
- P Lai, S Liao, J Jou. Transcaruncular approach for the management of frontoethmoid mucoceles. Br J Ophthalmol 2003. [Google Scholar]
- A Nemet, P Martin. The Lateral Triangle Flap—A New Approach for Lateral Orbitotomy. Orbit 2007. [Google Scholar] [Crossref]
- KS Moe, S Jothi, R Stern, HG Gassner. Lateral Retrocanthal Orbitotomy. Arch Facial Plast Surg 2007. [Google Scholar] [Crossref]
- P Pillai, M Lubow, A Ortega, M Ammirati. Endoscopic Transconjunctival Surgical Approach to the Optic Nerve and Medial Intraconal Space: A Cadaver Study. Neurosurgery 2008. [Google Scholar] [Crossref]
- PT Finger. Minimally invasive anterior orbitotomy biopsy: Finger's aspiration cutter technique (FACT). Eur J Ophthalmol 2012. [Google Scholar] [Crossref]
- T Lyson, A Sieskiewicz, M Rogowski, Z Mariak. Endoscopic lateral orbitotomy. Acta Neurochirurgica 2014. [Google Scholar] [Crossref]
- Nedal Hejazi. Frameless image-guided neuronavigation in orbital surgery: practical applications. Neurosurg Rev 2006. [Google Scholar] [Crossref]
- NR Miller, N Agrawal, JJ Sciubba, AP Lane. Image-Guided Transnasal Endoscopic Resection of an Orbital Solitary Fibrous Tumor. Ophthal Plast Reconstr Surg 2008. [Google Scholar] [Crossref]
- D W Kim, S R Choi, S H Park, S H Koo. Versatile use of extended transconjunctival approach for orbital reconstruction. Ann Plast Surg 2009. [Google Scholar]
- C S Lee, J S Yoon, S Y Lee. Combined transconjunctival and transcaruncular approach for repair of large medial orbital wall fractures. Arch Ophthalmol 2009. [Google Scholar]
- S Hamed-Azzam, D H Verity, G E Rose. Lateral canthotomy orbitotomy: a rapid approach to the orbit. Eye 2018. [Google Scholar] [Crossref]
- JG Camara, LT Nguyen, JP Fernandez-Suntay, GF Nardin, AS Sua. The Use of a Computer-Assisted Image-Guided System (InstaTrak) in Orbital Surgery. Ophthal Plast Reconstr Surg 2001. [Google Scholar] [Crossref]
