- Visibility 64 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijooo.2020.054
-
CrossMark
- Citation
Study of anterior chamber angle: Gonioscopy and ultrasound biomicroscopy
- Author Details:
-
Arpita Patel
-
Ashish Bhojak *
-
Hitesh Trivedi
Introduction
Gonioscopic evaluation of the anterior chamber angle is considered as gold standard of the diagnostic protocol of all eyes with glaucoma. Gonioscopy is a subjective test so there are interobserver variation is observed and also quantifaction of results is difficult.
In recent years, Ultrasound Biomicroscopy (UBM) has been used widely to evaluate the anterior chamber angle and the anatomical configuration of anterior segment particulary angle structures.
UBM technology has advantage of high image resolution so accurate identification of angle structures is possible. UBM provides accurate angle parameters measurement and quantification of data.
Still in practice, Gonioscopy has been the gold standard investigation for diagnosing open or narrow angle glaucoma classification and management but, it has limitation like its inability to measure anterior segment structures in extreme periphery of the angle. The angle opening in degrees is difficult to measure because of anatomical variations in angle structures and iris configuration. UBM provides indepth analysis in diagnostic dilemmas with reproducible, reliable results.
Materials and Methods
Our study is one year prospective and randomized, observational study with sample size of 100 patients (200 eyes).
Permission from ethical committee has been taken, then patients attending Ophthalmology OPD at tertiary eye care institute over period of 1 year are enrolled for study.
We have included patients attending Ophthalmology OPD between age group of 40 to 70 years with normal fundus examination and with normal Intraocular pressure (IOP). We have included all clinically suspected narrow angle patients.
We have excluded patients below 40 years of age and above 70 years of age. Patients with any ocular inflammation are also excluded. We have also excluded Patients with history of ocular trauma or laser procedures, intraocular surgery, Patients having corneal degenerations or haziness, Patients with raised IOP (intraocular pressure) or on pilocarpine eye drops.
Methods
Both eyes of 100 patients have been enrolled for study and written informed consent have been taken. Detailed ophthalmic evalauation has been done which included BCVA, detail slit lamp examination,transparency of cornea to rule out corneal degeneration/ haze/edema, pupillary reaction, lens changes ,anterior chamber evaluation for depth or any abnormal contents.
This was followed by grading of the Anterior chamber by using van-Herick’s technique. In this technique, the peripheral anterior chamber depth and corneal thickness is compared for grading of anterior chamber.
Fundus examination by direct and indirect ophthalmocsopy was done. History of systemic illness like hypertension, diabetes etc. and family history of glaucoma also taken carefully. Intraocular pressure measurement of all eyes done using Goldmann applanation tonometry.
Gonioscopy
Zeiss 4 mirror goniolens is used for Gonioscopic examination of angle of anterior chamber.
Gonioscopic technique
After Briefly explaining the procedure to the patient, in semi darkened room procedures were performed. Cleaning and sterilising the front (curved) surface of the goniolens done, after instillation of topical anaesthetic eye drops (0.5% proparacine) - Under slit-lamp visualization the lens is placed directly on centre of the cornea with only gentle contact is (excessive pressure will distort angle structures). Each quadrant of the angle is visualized with the opposite mirror. Care is taken to avoid light beam to pupil. The slit light beam used skillfully by examiner which is particularly helpful in grading angle width.
-Then angle graded according to Shaffer’s grading. [1]
|
ACA* in degree |
ACA grade |
Angle status |
Visible structures |
|
0 |
0 |
Close |
No structures visible |
|
≤10 |
1 |
Extremely narrow |
Schwalbe’s line |
|
11-19 |
2 |
Narrow |
Trabecular meshwork |
|
20-34 |
3 |
Open |
Scleral spur |
|
35-45 |
4 |
Wide open |
Ciliary bosy |
Ultrasound biomicroscopic evaluation done of same patients for angle measurement and anterior segment evaluation.
The examinations were performed using the UBM 840 instrument (Humphrey—Zeiss, USA) with a 35-MHz transducer probe. UBM imaging was done by the same ophthalmologist, and the examination was performed with the subject in supine position with eyes wide open. Care to be taken to avoid direct contact of probe with eye to prevent corneal injury. So The specially designed ocular cup filled with saline or 2% methyl cellulose was used Under topical anesthesia (0.5% proparacaine). Standard room illumination was maintained, and a randomly selected eye of the subject was imaged with radial scans at the 3, 6 and 9, 12 o’clock positions to obtain images centered over the limbal region; perpendicular scans centered over the pupil were also obtained. Three anterior segment parameters were measured on these images using a special caliper by the examiner. Anterior chamber details and anterior chamber angle like Parameters measured. The anterior chamber angle (ACA) is the trabecular iris angle. Precise measurement of the angle was done by UBM and graded according to Shaffer’s grading.
Lastly the ability of gonioscopy and UBM for accurate measurement of the angle of anterior chamber was assessed. The patients were divided according to the angle grading following gonioscopy and UBM and then compared.
Results
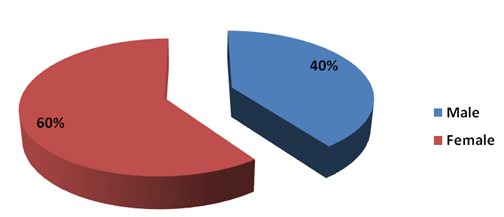
Our study included 100 patients among which 40 were males and 60 were females (200 eyes of the patient were examined).
Gonioscopic evaluation
Gonioscopy was done on all 200 eyes using ziess 4-mirror gonioprism and the angles of all the four quadrants were graded according to Shaffer’s grading.
|
|
Superior angle |
Inferior angle |
Temporal angle |
Nasal angle |
||||
|
|
Right eye |
Left eye |
Right eye |
Left eye |
Right eye |
Left eye |
Right eye |
Left eye |
|
Grade 1( no. of Pt) |
0 |
0 |
1 |
1 |
4 |
2 |
13 |
7 |
|
Grade 2 (no. of Pt) |
41 |
36 |
16 |
13 |
15 |
11 |
24 |
22 |
|
Grade 3 (no. of Pt) |
35 |
50 |
51 |
59 |
48 |
57 |
41 |
31 |
|
Grade 4 (no. of Pt) |
24 |
14 |
32 |
27 |
33 |
30 |
22 |
40 |
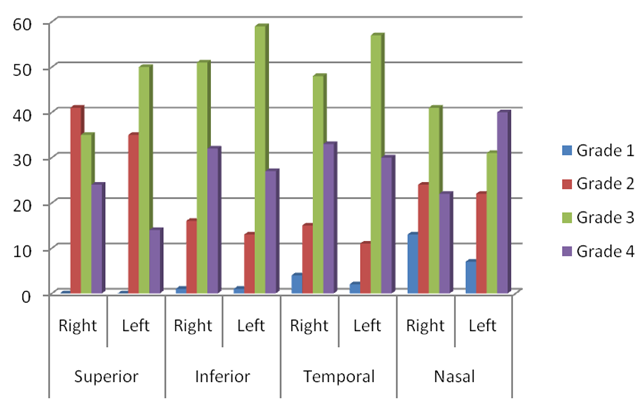
• Gonioscopy findings of Right eye suggestive that
-In superior angle 0 patients have grade 1 angle, 41 patients have grade 2 angles, 36 patients have grade 3 angle, 23 patients have grade 4 angle.In inferior angle 1 patient have grade 1 angle, 16 patients have grade 2 angle, 51 patients have grade 3 angle, 32 patients have grade 4 angle.In Temporal angle 4 patients have grade 1 angle, 15 patients have grade 2 angle, 48 patients have grade 3 angle, 33 patients have grade 4 angle.In Nasal angle 13 patients have grade 1 angle, 24 patients have grade 2 angles, 40 patients have grade 3 angle, 23 patients have grade 4 angle.
• Gonioscopy findings of Left eye suggestive that
- In superior angle 0 patients have grade 1 angle, 36 patients have grade 2 angles, 50 patients have grade 3 angle, 14 patients have grade 4 angle.In inferior angle 1 patient have grade 1 angle, 13 patients have grade 2 angle, 59 patients have grade 3 angle, 27 patients have grade 4 angle. In Temporal angle 2 patients have grade 1 angle, 11 patients have grade 2 angle, 57 patients have grade 3 angle, 30 patients have grade 4 angle.In Nasal angle 7 patients have grade 1 angle, 22 patients have grade 2 angles, 31 patients have grade 3 angle, 40% patients have grade 4 angle.
So final result ,Gonioscopy findings suggestive of 3.5% patients have grade 1, 22.25% patients have grade 2, 46.50% patients have grade 3, 27.75% patients have grade 4.
|
|
Gonioscopy (%) |
|
Grade 1 |
3.50% |
|
Grade 2 |
22.25% |
|
Grade 3 |
46.50% |
|
Grade 4 |
27.75% |
|
|
100.00% |

Ultrasound biomicroscopic evaluation
UBM evaluation of all 200 eyes were done for measurement of angle of anterior chamber using 3 point technique.
|
|
Superior angle |
Inferior angle |
Temporal angle |
Nasal angle |
||||
|
|
Right eye |
Left eye |
Right eye |
Left eye |
Right eye |
Left eye |
Right eye |
Left eye |
|
Grade 2 (no. of Pt) |
2 |
1 |
1 |
2 |
2 |
2 |
10 |
7 |
|
Grade 3 (no. of Pt) |
49 |
52 |
28 |
31 |
26 |
24 |
39 |
28 |
|
Grade 4 (no. of Pt) |
49 |
47 |
71 |
67 |
72 |
74 |
51 |
65 |
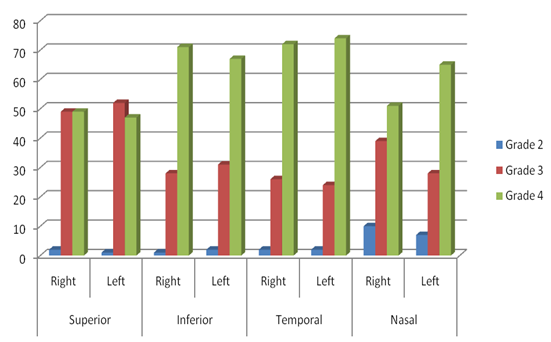
• UBM findings of Right eye suggestive that
-In superior angle 0 patients have grade 1 angle, 2 patients have grade 2 angles, 49 patients have grade 3 angle, 49 patients have grade 4 angle.In inferior angle 0 patients have grade 1 angle, 1 patient have grade 2 angle, 28 patients have grade 3 angle, 71 patients have grade 4 angle. In Temporal angle 0 patients have grade 1 angle, 2 patients have grade 2 angle, 26 patients have grade 3 angle, 72 patients have grade 4 angle. In Nasal angle 0 patients have grade 1 angle, 10 patients have grade 2 angles, 39 patients have grade 3 angle, 51 patients have grade 4 angle.
• UBM findings of Left eye suggestive that
- In superior angle 0 patients have grade 1 angle, 1 patient have grade 2 angle, 52 patients have grade 3 angle, 47 patients have grade 4 angle.In inferior angle 0 patients have grade 1 angle, 2 patients have grade 2 angles, 31 patients have grade 3 angle, 67 patients have grade 4 angle. In Temporal angle 0 patients have grade 1 angle, 2 patients have grade 2 angle, 24 patients have grade 3 angle, 74 patients have grade 4 angle. In Nasal angle 0 patients have grade 1 angle, 7 patients have grade 2 angles, 28 patients have grade 3 angle, 65 patients have grade 4 angle.
|
|
UBM |
|
Grade 1 |
0% |
|
Grade 2 |
3.38% |
|
Grade 3 |
34.62% |
|
Grade 4 |
62% |
|
|
100% |
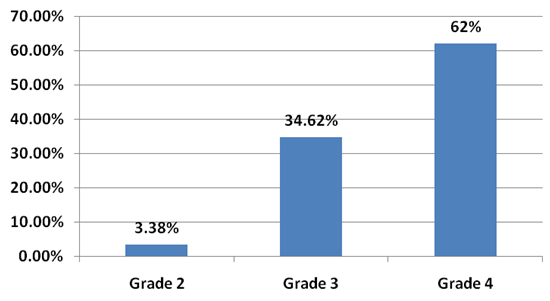
UBM finding suggestive 0% patients have grade 1, 3.38% patients have grade 2, 34.62% patients have grade 3 angle and 62% patients have grade 4.
Comparision of gonioscopy and UBM findings
|
|
Gonioscopy |
UBM |
|
Grade 1 |
3.50% |
0% |
|
Grade 2 |
22.25% |
3.38% |
|
Grade 3 |
46.50% |
34.62% |
|
Grade 4 |
27.75% |
62% |
|
|
100.00% |
100% |
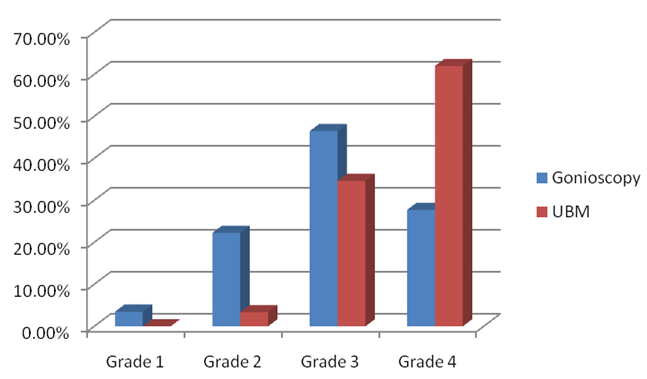
On comparision of angle grades of both gonioscopy and UBM findings, 3.5 % patient have grade 1 on gonioscopy while on UBM 0%, 22.25% patient have grade 2 on gonioscopy while on UBM 3.38%, 46.50% patient have grade 3 on gonioscopy while on UBM 34.62%, 27.75% patient have grade 4 on gonioscopy while on UBM 62%.
|
UBM Grading |
Gonioscopic Grading |
|||
|
Grade 1 |
Grade 2 |
Grade 3 |
Grade 4 |
|
|
Grade 1 |
0.00% |
0.00% |
0.00% |
0.00% |
|
Grade 2 |
77.78% |
1.69% |
1.07% |
0.00% |
|
Grade 3 |
22.22% |
96.61% |
25.67% |
1.80% |
|
Grade 4 |
0.00% |
1.69% |
73.26% |
98.20% |
Discussion
Grading of angle width with gonioscopy is widely used method in glaucoma assessment protocol. The Shaffer grading system[1] is most commonly used method to classify between open angle and narrow angle glaucoma. This system determines the approximate angle in degrees.
Gonioscopy is a subjective test, so accurate quantification is not possible in all cases. The role of the UBM as a newer quantitative tool[2] has been studied by various authors.
According to UBM finding among the 100% of the eyes which belonged to the grade 3 of the Shaffer’s grading only 34.62% eyes were included in grade 3 with gonioscopic evaluation whereas the remaining of them i.e. 65.38% were graded under grade 2. Similarly following UBM the 100% eyes which belonged to grade 4 only 24.4% of the eyes belonged to grade 4 after gonioscopic evaluation where as remaining 70% were included in grade 3 and 5.6% were included in grade 2.
The study summarizes that gonioscopy could detect only 33.3% of the total grade 3 angles accurately whereas remaining 66.7% could not be detected by gonioscopy and were falsely grouped under grade 2 which was overdiagnosis of the narrow angles and hence shown to belong to occludable angles inspite of the angle measurement being more than >25.
Our study shows that some amount of estimation of angle depth by gonioscopy is inaccurate in slit-like and grade 1 angles, whilst estimation of grades 2 and 3 is fairly accurate. These errors result in the wrong classification of open angles as occludable, which is possibly an indication that subjective gonioscopy is not a reliable method to differentiate occludability from nonoccludability. It also results in over- diagnosis of occludable angles.
UBM provides indepth examination into the AC angle structures, anatomical variations & allows for detailed imaging of the ciliary body.[3], [4] UBM is also useful in conditions like eyes with corneal edema or corneal opacification where gonioscopic assessment is difficult.
In open-angle glaucoma, UBM can be used to assess the configuration of the peripheral iris, and to evaluate the iris insertion.[5] anatomical variation like anterior insertion of the iris or an anteriorly displaced ciliary body also can be detected.
The study done by Narayanswamy et al[6] which proved that UBM provides a more quantitative measurements in glaucoma evaluation . UBM was able to measure angle more accurately as compared to gonioscopy. Gonioscopy lead to over diagnosis of occludable angles which might lead to diagnosis of angle closure glaucoma.
Ultrasound biomicroscopy and more recently anterior segment optical coherence tomography are imaging modalities that can be used to obtain two-dimensional images of the angle and surrounding structures. Ultrasound biomicroscopy has the advantage of being able to illustrate the ciliary body and therefore give clinicians information on nonpupil block mechanisms of primary angle closure[7] and also diagnose other abnormalities such as cyclodialysis clefts. With the UBM, examination of the angle structures[8] in which iris, ciliary body, and scleral spur details can be identified easily.
The UBM can be used successfully to measure and evaluation of angle structures in glaucoma with added advantage of ability to visualize ciliary body, pars plana and zonules.
Hence, the UBM and gonioscopy both are useful in aid to glaucoma evaluation with few advantages and disadvantages of each tool.
Conclusion
Our study shows that some amount of estimation of angle depth by gonioscopy is inaccurate in slit-like and grade 1 angles, whilst estimation of grades 2 and 3 is fairly accurate. These errors result in the wrong classification of open angles as occludable, which is possibly an indication that gonioscopybeing subjective, is not a reliable method to differentiate occludable angle from nonoccludable angle.
Gonioscopy may be associated with measurement errors like artificially opening the angle or closing due to how the lens is placed on the eye. Reproducibility of gonioscopy has only rarely been studied in small samples of patients, with moderate agreement reported.
UBM can be used to measure the accurate anterior chamber angle in degrees, to assess the configuration of the peripheral iris, and to evaluate the iris insertion in relation to the trabecular meshwork.[3] Imaging of the anterior segment structures is possible even in eyes with corneal edema or corneal opacification where gonioscopy is not possible. Iris contour evaluation by UBM[9] gives accurate angle width measurement and this explains the misjudgement in goniscopic estimation, especially in the occludable angles, where the contours tend to be more convex.
Ultrasound biomicroscopy has the advantage of being able to illustrate the ciliary body and therefore give clinicians information on nonpupil block mechanisms of primary angle closure and also diagnose other abnormalities such as cyclodialysis clefts. Inspite of this, gonioscopy is helpful to differentiate appositional from synechiael angle closure and extent of preipharal anterior synechiaes. So, we recommend use of UBM for accurate grading of angle in every suspected narrow angle patients by van herick’s method on slit lamp examination.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- RN Shaffer. Primary glaucomas. Gonioscopy, ophthalmoscopy and perimetry. Trans Am Acad Ophthalmol Otolaryngol 1960. [Google Scholar]
- S Mohan, S Vengayil, A Aggarwal, V Gupta, R Sihota. Clinical Applications of Ultrasound Biomicroscopy in Glaucoma. J Curr Glaucoma Pract 2007. [Google Scholar]
- S Kaushik, R Jain, SS Pandav, A Gupta. Evaluation of the anterior chamber angle in Asian Indian eyes by ultrasound biomicroscopy and gonioscopy. Indian J Ophthalmol 2006. [Google Scholar] [Crossref]
- N Wang, T Ye, M Lai, Y Ou, M Zeng, C Yang. Comparison of results of chamber angle examination ultrasound biomicroscopy and Gonioscopy. Zhonghua Yan Ke Za Zhi 1999. [Google Scholar]
- K Syril, Yariv Dorairaj, Jeffrey M Gerber, Liebmann. Agreement between Gonioscopy and Ultrasound Biomicroscopy in Detecting Iridotrabecular Apposition: Yaniv Barkana. Arch Ophthalmol 2007. [Google Scholar]
- A Narayanaswamy, L Vijaya, B Shantha, M Baskaran, AV Sathidevi, S Baluswamy. Anterior Chamber Angle Assessment Using Gonioscopy and Ultrasound Biomicroscopy. Japanese J Ophthalmol 2004. [Google Scholar] [Crossref]
- CS Garudadri, V Chelerkar, R Nutheti. An Ultrasound Biomicroscopic Study of the Anterior Segment in Indian Eyes with Primary Angle-Closure Glaucoma. J Glaucoma 2002. [Google Scholar] [Crossref]
- I Hiroshi, L Jeffrey, R Robert. Quantitative assessment of the anterior segment using ultrasound biomicroscopy. Curr Opin Ophthalmol 2000. [Google Scholar]
- F Mircea, F Andrei, D Carmen, N Miruna. Old and new in exploring the anterior chamber angle Moisescu Raluca. Rom J Ophthalmol 2015. [Google Scholar]
