Introduction
Hidrocystomas are rare, benign, cystic lesions of the skin often found on the head and neck region and typically occurs on the face in adults between 30 and 70 years of age. Clinically eccrine hidrocystoma occur in whites, adult women. They are usually small, of size 1 to 6 mm in diameter and presents as single or multiple tense thin-walled cyst lesions, predominantly over periorbital and malar region.1 The cysts when multiple, are found typically on the face; when solitary, they are found on the neck, chest, and trunk. In multiple cystic lesions, the differential diagnosis is with miliaria crystallina, steatocystoma multiplex and eruptive vellus hair cysts. If solitary, the differential diagnosis is apocrine cystadenoma, cystic basal cell carcinoma, and cutaneous ciliated cysts.
Apocrine hidrocystomas affect older adults with equal sex incidence.2 It is due to the adenomatous cystic proliferation of apocrine glands, typically occur as fluid filled solitary lesion rarely as multiple lesions.3 The lesion is usually of a diameter of 3 to 15 mm and mostly on the head and neck and along the eyelid margin specifically near inner canthus.4 Other rare sites documented are axilla, penis and anus.5 The clinical differential diagnosis is basal cell carcinoma and certain melanocytic lesions such as blue nevi.
Case Summary
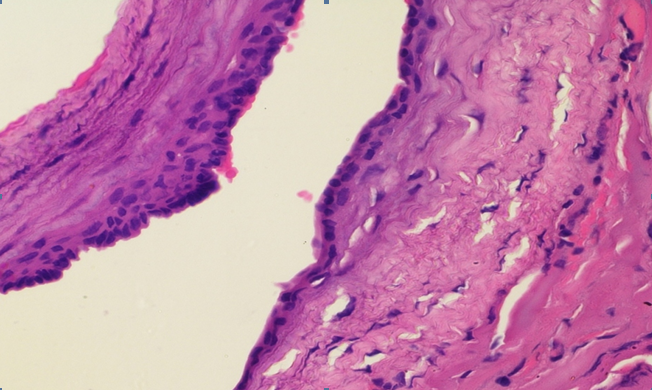
A 60 year old female presented to ophthalmology clinic with a swelling over left lower eyelid for the past 4 months. Examination disclosed a cystic fluid filled skin coloured lesion and measured approximately 0.6×0.3 cm with fluctuation test positive. There was no proptosis and no change in the lesion with the Valsalva maneuver. The patient denied of any diplopia, vision loss, or any other lesion on her face or body. Her review of other systems, personal and family histories were all normal or noncontributory. She took no medications and had no known allergies to medications. Ultrasound biomicroscopy showed a fairly circumscribed echolucent mass suggestive of a cyst with numerous internal echo impedances. On the basis of the clinical evidence, solitary eccrine hidrocystoma was diagnosed and the patient was kept on topical atrophine sulphate 1% in aqueous solution three times a day. However, she complained of intolerance to blurred vision. The lesion was subsequently excised with a good response. Microscopically, tissue section showed foci of stratified squamous epithelium with an underlying cystic cavity lined by 1-2 layers of small cuboidal epithelial cells (Figure 1, Figure 2). Overall morphology was consistent with eccrine hidrocystoma. Our patient has completely recovered without any recurrence during follow up after 6 months.
Discussion
Hidrocystoma also known as sudoriferous cyst, is an eyelid tumor which originates from apocrine or eccrine sweat glands.6 The eccrine type tends to produce watery secretions whereas the apocrine type tends to produce oily, foamy secretions. The most acceptable pathological cause is that the apical part of cellular cytoplasm is decapitated in the apocrine type (decapitation), while it remains intact in eccrine (exocytosis) glands.7
Eccrine hidrocystoma is a cutaneous lesion that occurs predominantly on the face.8 Most prevalent form of eccrine hidrocystoma is solitary type, also known as Smith type and when multiple, it is the robinson type of hidrocystoma. The individual lesion of multiple type is similar to Smith type except that they are smaller in size. 9 It presents as dome shaped cystic swelling usually involving the mid-dermal to superficial layers of eyelid skin and not the eyelid margin, the lower half of the upper eyelid pretarsal skin, or the pretarsal lower eyelid skin due to the absence of eccrine glands. On an average they measure 4 mm in the largest dimension. It is rare for eccrine hidrocystoma of the eyelid to be larger than 10 mm. Mostly occur during hot, humid weather with increase in size and number whereas no evidence of seasonal variations is seen with apocrine hidrocystoma. It usually contains a single cystic cavity composed of one or two layers of cuboidal cells. Sometimes the content of the cysts has a brownish color giving a clinical appearance similar to the blue nevus or melanoma due to secretion of lipofuscin secreted by the neighbouring cells.
The apocrine hidrocystoma lesions are unilocular or multilocular cystic structures containing a clear or brownish fluid. Apocrine glands are restricted to the eyelid margins and canthi where the cysts were located. Histologically, the cyst lining consists of a layer of high columnar cells with abundant eosinophilic, granular cytoplasm and a round, basally located nucleus oftenly with "Decapitation" secretion indicated by apical snouts. Papillary structures, if present, are lined by apocrine i.e., secretory epithelium. These projections are vascular connective tissue, which appear in the lumen of the cyst as an outgrowth extension from the wall of the cyst.4 Rarely, the lining epithelium may form a cribriform or microcystic pattern. If excessive, the epithelial proliferation may be similar to hidradenoma papilliferum or syringocystadenoma papilliferum.
Histochemically, eccrine hidrocystoma stain positive for S100 protein as well as CK7 positivity in luminal cells (solitary type), whereas apocrine hidrocystomas give negative staining as the cyst and epidermis do not communicate, and hence, the periodic acid-Schiff (PAS)-positive granules are not observed. Apocrine hidrocystoma shows positivity for GCDFP15, suggesting origin from glandular secretory spirals.
Both medical and surgical treatment modalities are available. Medically, they can be treated with topical application of 1 percent atropine sulfate ointment or with an oral anticholinergic agent, glycopyrrolate which prevents hyperhidrosis.10 Surgical excision of the cyst en mass without rupturing the wall of the cyst is the preferred modality for solitary lesion and not for the elimination of multiple lesions because of their number and location. Intralesional botulinum toxin A offers a novel treatment for patients in multiple hidrocystomas that have failed other therapies. Other treatment modalities included are cauterisation and electrodessication, carbon diaoxide vaporization and laser.