Introduction
Most cases of ocular blindness and disability not only in India but also worldwide could be accounted due to ocular trauma. Ocular trauma often causes traumatic cataract leading to morbidity both in context of visual and vocational morbidity inspite of tremendous advancement in field of diagnosis and management.
Up to one-fifth of total indivisuals are going to experience minor or major ocular trauma at some point in their lives. Most common age group being affected are young population and men are affected more than the females. According to a study done by World Health Organization up to 55 million eye injuries occur annually worldwide, and up to 1.6 million people become blind due to eye trauma.1
The pathophysiology of cataract following trauma is due to partly to mechanical effect of injury on lens fibre and mostly due to entrance of aqueous due to damage of capsule, either secondary to impairement of its semipermeability or often result of actual tear. It occurs at posterior pole which is the thinnest portion of capsule covering lens. sometime tear may seal by plugging of iris, at first with fibrin and subsequently by subcapsular epithelium proliferation.In these cases where tear is self-limiting opacity remain stationary. In other scenario where tear is open opacity progress to involve entire lens. visual outcome after trauma depends on subsequent involvement of by anterior and posterior segment depending on the force of trauma.2, 3 It also depends on the severity of the trauma, prior visual acuity, pupillary reflex response, and depth of globe penetration The most typical appearance of traumatic cataract after concussion is a rosette-shaped cataract.
Methods and Materials
A prospective hospital based study was conducted in our Navodaya medical college and research centre Raichur from August 2018 to July 2019. The study included all the patients of ocular injury who were affected from blunt and penetrating trauma and involving only anterior segment. All cases were confirmed before admission from casulaty or from OPD, that they are the case of cataract following trauma other causes were excluded.
Mode of injury
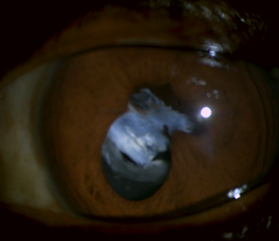
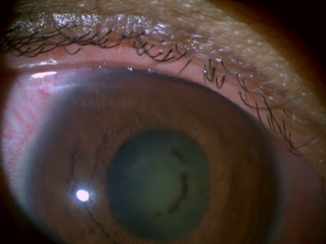
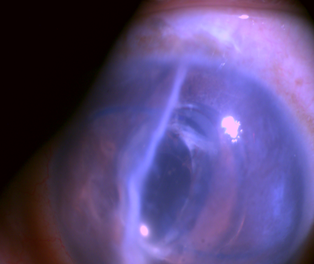
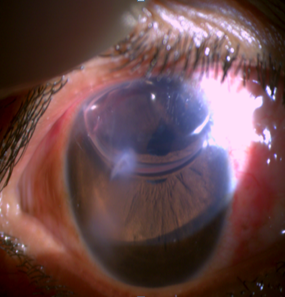
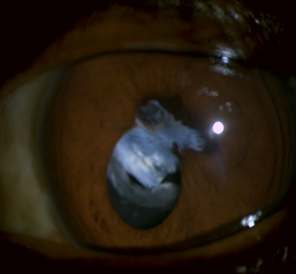
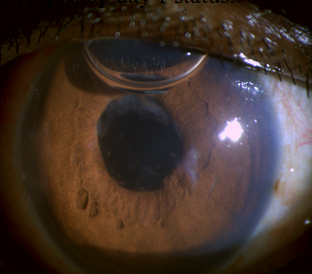
Once it is confirmed a as case of traumatic cataract then it should be determined whether it is secondary to penetrating or blunt trauma. Blunt injury is one which is caused by blunt object like (cricket ball, champagne cork etc.)(Figure 2, Figure 3) and penetrating trauma is one which has entry wound but not exit wound, caused by object like (iron rod, wooden stick thorn etc.) (Figure 4, Figure 5) After the mode of injury IOP should be determined if low it always raise the suspicion of open globe injury; however in some cases the wound is self-sealing and IOP may be normal which is confirmed by Siedel’s test which is done at the site of wound first penetrating trauma should be ruled out once it is done the status of posterior segment is seen by ultrasound biomicroscopy. If penetrating trauma is present use of topical medication or instruments that coming in contact with intraocular tissue should be avoided as it interferes with integrity of globe. Patients who were cooperative and willing for the surgery were included after taking the consen.
Trauma history uncertain
Impacted intraocular foreign body ocular damage beyond recovery traumatic removal of lens. Complicated cataract, congenital cataract. Retinal detacement, vitreous haemorrhage any other causes involving posterior segment.
Preoperative assessment included detailed history taking about modes of injury (penetrating or blunt) and causative agents (stone, iron rod, glass piece cricket ball, fist) and severity of injury. After history general examination was done. Once the general condition of the patients are established it follows local examination which included:
Best corrected visual acuity (BCVA) for distant and near both, torch light and detailed slit lamp examination of the anterior segment, tonometry, gonioscopy, wet retinoscopy, fundus examination with the direct and indirect ophthalmoscope, keratometry (in case of corneal opacification opposite eyes were used), Intraocular lens power calculation and Bscan was done. Other relevant examinations should also be done and routine laboratory investigations were also done before surgery.
Before moving on the surgical procedure integrity of globe has to be restored then inflammation has to be subsided by systemic steroids and relevant medication. surgery was done under local anaesthesia, peribulbar block was given over massaging should be avoided as it aggravates zonular dialysis SMALL INCISION cataract extraction (SICS) with primary posterior chamber intraocular lens (PCIOL) implantation was done. In patient with corneal tear cataract removal with IOL implantation was done in two settings. In first setting corneal tear was repaired with 10-0 monofilament suture and in second setting cataract extraction with IOL implantation is done. In mild lenticular subluxation with partial zonulolysis SICS with PCIOL implantation was done depending upon the integrity of Posterior capsule. If posterior capsular bag integrity is good then a 1-piece PMMA IOL was implanted in bag.
If posterior capsule integrity is compromised and if enough of the anterior capsule remains to support and if proper anterior capsulorhexsis was possible then a 3-piece PMMA IOL implantation was placed in ciliary sulcus. If posterior capsule was severely compromised and more than half zonulolysis then secondary IOL placement preferably iris claw lens was done. In few cases where cataract was densely attached to posterior capsule, posterior capsulotomy was done and IOL was placed in the bag. Data was analysed with regard to relationship between different causes of trauma and, resulting injury and final visual outcome achieved with surgical technique. Patients were subsequently followed up at 1 week, 1 and 6 month and best corrected visual acuity was recorded.
Results
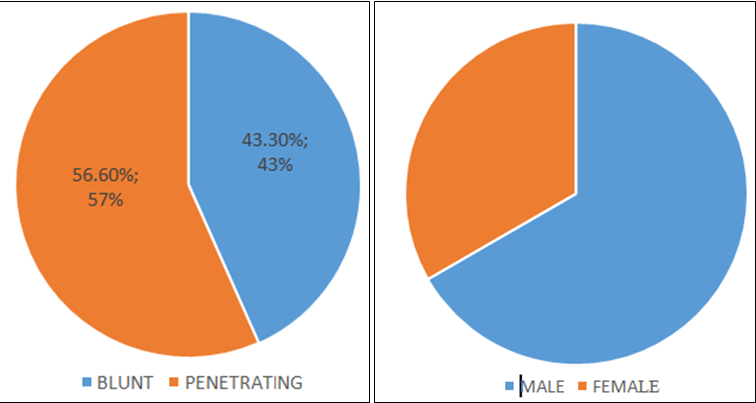
We included total of 30 patients in our study in which 56.6% sustained penetrating trauma while 43.3% were imposed with blunt injury (Figure 1). Out of 30 patients, 20 (70%) were males and 10 (30%) were females. Young males suffered more from penetrating trauma than blunt trauma (56.6% vs 43.3%) (Figure 1). The causative agents could be of varied variety like champagne cork, fist stone, wooden stick, metal object etc. The common cause for penetrating injury being wooden stick while blunt often occur following injury with stone. [Table 2] show corrected visual acuity on admission in case of blunt and penetrating trauma. Out of 13 blunt trauma cases, 15.3% of patients had visual acuity <6/60 while 61.13% had visual acuity >6/18. Out of 17 penetrating trauma cases, 23.52% of patients had visual acuity <6/60 while 35.02% had visual acuity >6/18. Our study concluded most common cause for blunt injury is stone while the most common cause for penetrating injury is wooden stick.
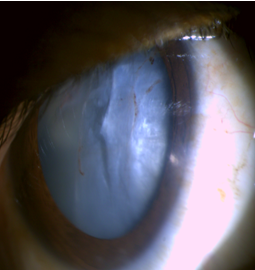
In our study we found that corneal involvement was most common associated ocular damage (Figure 6, Figure 7) and it was found that it is one the most common cause of reduced visual acuity following penetrating trauma.
Associated ocular injuries (Fig. 1-4)
Before and after surgery (Fig. 5-8)
Discussion
Our study out of 30 cases of traumatic cataract, 56.6% sustained penetrating trauma and 43.32% had blunt trauma. Our result were consistent with Daljit Singh et al who also found in their study penetrating trauma the leading cause of trauma is that fifty percent of total trauma cases.4 in our we also reorted that male were affected 66.6% as compared to female 33.3% and this result was consistent with Srivastava et al.5 and other studies.6, 7, 8, 9 The most common cause for blunt injury is stone while the most common cause for penetrating injury is wooden stick and this was consistent with Tewari et al and Krishnan et al.10 Our study revealed that satisfactory visual outcome in most of the patients with traumatic cataract could be achieved after cataract removal and intraocular lens implantation.
Conclusion
Our study concludes that the younger males common sufferer than female due their more involvement in outdoor activities. Penetrating injuries being more frequent than the blunt injury. Blunt injury has better visual outcome than penetrating injury because structural integrity is maintained. In case Penetrating trauma BCVA is less due to associated ocular injury, more of corneal involvement. It also depend various factor ranging from force of trauma affecting anterior and posterior segment (Figure 6, Figure 8), severity of damage, any preceding ocular conditions, proper and timely medical and surgical management of these cases, and management of post operative complications and regular followup.