Introduction
Pterygium is a triangular fibrovascular subepithelial ingrowth of degenerative bulbar conjunctival tissue over the limbus onto the cornea.1 Pterygium mostly causes "with the rule astigmatism" that is: vertical meridian is more steeper than horizontal meridian as pterygium generally encroaches the cornea from the nasal side in a horizontal direction at first which causes the H meridan to flatten but gradually when the pterygium progresses it leads to irregular astigmatism.2
Grading of pterygium according to Youngson R.M3
Grades of pterygium
Aims and Objectives
Review of Literature
Three topographic properties of the cornea are important to its optical function: the underlying shape, which determines its curvature and hence its refractive power.4
The development of a pterygium can lead to significant astigmatism. A pterygium generally causes localized flattening central to the apex of the pterygium.5 As this flattening is along the horizontal meridian, it usually causes with-the-rule corneal astigmatism.6 The vertical corneal meridian is steep in younger adults. This reduces with age and tends to give rise to against the rule astigmatism in later years.7 Fong et al. in 1998 observed that pterygium excision usually induces a reversal of pterygium-related corneal flattening.8
Pterygium is described as an active, invasive and inflammatory process where subconjunctival tissue undergoes elastotic degeneration and proliferates as fibrovascular granulation tissue under the epithelium, which encroaches onto cornea.9 Pterygium is an acquired, chronic and degenerative disease. The exact etiology of pterygium is still unknown. But, it is more common in people living in hot dry climates. Due to prolonged effect of environmental factors such as exposure to sunlight, dry heat, high wind and abundance of dust. It is more common in males than female because of long outdoor work. Pterygium usually occurs on the nasal side of bulbar conjunctiva between inter palpebral fissures. It can also occur at temporal side of bulbar conjunctiva but it is more commonly seen along with nasal pterygium. Both Nasal and temporal pterygium in one eye is called as Double Pterygium. Pterygium can be unilateral or bilateral, but asymmetrical. It is common in old age. Pterygium presents mainly with symptoms like foreign body sensation, irritation, cosmetic reason, impairment of vision as it encroaches onto cornea and causes astigmatism. Pterygium can progress and can reach up to pupillary margin or beyond that covering pupil and causes visual axis obstruction of visual axis.10
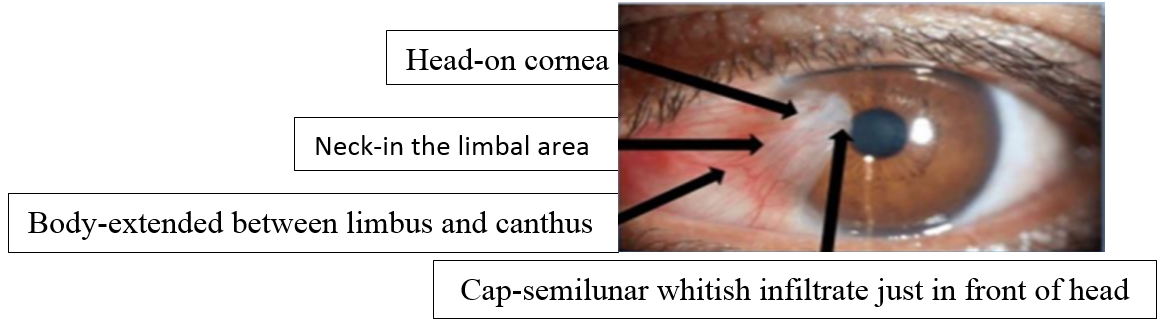
Flattening was seen in the horizontal meridian, which was associated with astigmatism. The exact mechanism of flattening is not clear. It is thought to be caused by the formation of tear meniscus between the corneal apex and the elevated pterygium, causing an apparent flattening of the normal corneal curvature. Pterygium induces significant astigmatism which may be either ‘with-the-rule’(WTR) or ‘against-the-rule’ (ATR). The mechanisms explaining the astigmatism are: the tractional force of contractile elements within the pterygium lead to mechanical distortion and flattening of the cornea in its horizontal meridian leading to hypermetropic WTR astigmatism. Pterygium induced with-the-rule corneal astigmatism is hemimeridonal on the side of the pterygium resulting in a localized flattening of the cornea central to the leading apex. The localised pooling of tears at the advancing edgehead of the pterygium is also responsible for corneal flattening.Pterygium results in high corneal astigmatism, which decreases following an excision. Pterygium can be divided into 4 parts:- 1) Head: - Apical part of pterygium on the cornea. 2) Neck: - lies between head and body onto the limbus. 3) Body: - It represents as main part of the pterygium lying over the sclera and extending from the canthal side of bulbar conjunctiva. 4) Cap: - It is present just in front of the head. It can be of two types, few whitish infiltrates seen just in front of head of pterygium is called “Fuch’s spots”, “Fuch’s islands” or “Fuch’s islets” and another is “Stocker’s line” - an iron deposited line in front of head of pterygium.
According to the progression pterygium is of two types:- (1) PROGRESSIVE: - It is described as thick, fleshy and vascular pterygium with fuch’s spot. (2) REGRESSIVE OR ATROPHIC: - thin, atrophic, attenuated pterygium with very little vascularity. Stocker’s line is present in this type of pterygium. This pterygium ultimately regresses and becomes more atrophic and membranous but it never disappears.11
Pterygium more frequently occur on nasal side than temporal side. The bulbar conjunctiva of temporal side of the cornea is situated below the lacrimal gland so it is less prone to drying as it is bathed by fresh tears so the relative rarity of pterygium is in the temporal side. Rarity of temporal side of pterygium can be explained by aqueous tear secretion but it does not explain mucin deficiency association.11 Pterygium present on the nasal side is an indication of the pathogenetic role of the solar light as light gets reflected from lateral wall of nose onto the nasal side of bulbar conjunctiva. Nasal pterygium can also be explained by noting that longer temporal eyelash of upper eyelid shade and filter sunlight falling on the temporal conjunctiva and cornea than on nasal side.12,13 Elliot explained that because of wind, drying tissue of the medial third of the palpebral aperture devitalizes which leads to actinic reaction to damage cornea and conjunctival layers.14 pterygium occurs more in dominant eye, probably due to the non-dominant eye is closed in intense sunlight.13
Different surgical options for pterygium are:
Bare sclera excision (d’ombrain)
Mitomycinc (mmc)
Pterygium excision with amniotic membrane transplant
Pterygium excision with conjunctivo-limbal autograft transplantation using fibrin glue
Pterygium excision surgery with conjunctivo -limbal autograft transplantation using sutures
Pterygium excision with conjunctivo-limbal autograft transplantation using patient’s own blood
Lamellar keratoplasty and excimer laser phototherapeutic keratectomy(are being studied
Out of all techniques conjunctival autografting is the best available option after pterygium excision to prevent recurrence.15,16,17,18 Study has compared sutureless glue-free versus sutured limbal conjunctival autograft in primary pterygium surgery in adults and showed sutureless glue-free limbal conjunctival autograft is safe, effective, economical and had greater patient satisfaction.18
Materials and Methods
A comparative study was undertaken where the refractive status of patients with pterygium pre-opreative and post operative with conjunctival autograft with suture and without suture was evaluated.
Study period
September to September-2019
Institute ethics committee clearance have been obtained before the start of the study.
Written and informed consent was obtained from all the patients.
Sample size
50 cases
Considering the average number of patient attending the OPD in D.Y. Patil medical college and having diagnosed pterygium being 2-3 cases per month :
The period of the study being 24 month, sample size was 50 cases.
Methodology
All patients included in the study were diagnosed to have pterygium induced astigmatism. Patients were explained about the study after which written and informed consent was taken about their participation in the study.
Following protocols were undertaken in each case:
Demographic factors like age, sex, occupation and address were recorded as per the attached proforma.
Complete ophthalmic and medical history was take
Visual acuity using Snellen’s chart.
Refractive status deduced
Keratometery observed for horizontal and vertical diameters corneal diopteric
Surgical technique.
Total of 50 cases of pterygium induced astigmatism were included in this study which were operated by pterygium excision and conjuctival autograft with suture or without suture.
Patients were examined on post operative day 1,7,21 for refractive status.
Statistical analysis
Data was entered in Microsoft Excel and statistical analysis was done using software EpiInfo or SPSS.
Quantitative data was analysed in terms of Means and Standard Deviation.
Qualitative data was analysed with appropriate test of significance like Unpaired T test and Paired T test.
Results
Total of 50 cases of pterygium induced astigmatism were included in this study. Out of which 25 patients were operated with conjunctival autograft without suture and 25 pateints were operated using conjunctival autograft with suture technique. These were following observations and results of the present study:
Table 1
| N | 50.00 |
| Mean | 2.52 |
| Std. Error of Mean | 0.15 |
| Std. Deviation | 1.06 |
| Range | 3.50 |
| Minimum | 1.00 |
| Maximum | 4.50 |
Size of pterygium (mm) Statistics
In present study mean size of pterygium tissue was 2.52 mm with standard deviation of 1.06 mm, with the highest 4.5 mm and lowest 1 mm.
In present study Grade 3 (44%) was most common followed by grade 2 (26%) followed by grade 4 (24%).
On application of spearman’s correlation, there was positive correlation between grade of pterygium and KV – KH (diopter) which was highly significant. It means as grade of pterygium increases, difference between KV – KH also increases (Spearman’s rho 0.482, p = 0.000)
Table 2
Keratometry readings in vertical (KV) and horizontal (KH) meridian pre-operatively and post-operatively
Table 3
Comparison of KV and KH pre-operatively and post-operatively
Table 3 statistics shows that, significant difference was seen in mean KV and KH pre-operatively, on post operative day 1 after pterygium excision surgery with conjunctival autograft with or without suture and on regular follow up (p = 0.000), such that KV(43.84 + 1.01 decreases to 43.08 + 0.72) decreases while KH (41.30 + 0.96 increases to 42.56 + 0.79) increases following surgery and serial follow up.
Table 4
Mean (KV minus KH) pre-operatively, on post operative day 1 and on regular follow up
Table 4 statistics shows that, mean (KV minus KH) pre-operatively, on post operative day 1 and on regular follow up was statistically significant (p = 0.000). (KV minus KH) decreases (2.55 + 1.14 reduces to 0.60 + 0.41) after pterygium excision surgery with conjunctival autograft with or without suture
Table 5
Change in refractive error pre-operatively and on post-operative day 1, 1 week, 3 week
Table 6
Change in spherical and astigmatism error pre-operatively and post-operatively
The present study shows that, mean spherical error (SE) (1.06 + 1.39) and astigmatic error (AE) (1.02 + 0.89) pre-operatively, on post operative day 1 and on regular follow up was statistically significant (p = 0.000). Spherical (0.08 + 0.23) and Astigmatic error (0.17 + 0.26) reduces significantly after pterygium excision surgery with conjunctival autograft with or without suture.
Table 7
Comparison of keratometry readings between two type of surgery
On application of unpaired t test, no significant difference was observed between mean vertical (KV) and horizontal (KH) or their difference (KV-KH) by two types of surgery (Pterygium excision with conjunctival autograft without suture or with suture) at various duration of study (p > 0.05). It mean in comparison between pre-operative and post-operative status there was equal reduction of KV, difference between KV & KH, increase in KH following two types of surgery.
Chart 3
Change different type of refractive errors among patients pre-operatively and post-operatively

Figure 7 shows that, simple myopic astigmatism (32%) was most common pre-operatively followed by compound hypermetropic astigmatism (28%). Post-operatively, 56% subjects were having no refractive error followed by simple myopic astigmatism (26%). Almost no change was seen in spherical refractive error where as astigmatic error was reduced or nullified.
Chart 4
Change in type ofastigmatism among patients pre-operatively and on regular follow uppost-operatively

Figure 8 shows that, with the rule astigmatism (58%) was most common pre-operatively followed by against the rule astigmatism (32%). Post-operatively, majority of the subjects that is (68%) subjects were having no astigmatism while only (14%) patients had against the rule astigmatism.
Figure 9 shows that, compound hypermetropic astigmatism was seen in most of the cases of grade 3 and 4 pterygium and simple hypermetropic astigmatism was seen in grade 2 pterygium. Grade 1 causes only simple myopic astigmatism.
Figure 10 shows that, after pteryguim excision surgery patients with grade 3 and grade 2 pterygium patients had drastic reduction in astigmatic error.
Comparing pre-operative and post-operative refractive error after pterygium surgery shows that, in grade 1 pterygium simple myopic astigmatic error almost remains same. In Grade 2, 3 pterygium patients had no refractive error to mild simple myopic astigmatic error but compound hypermetropic astigmatism is completely nullified.
Discussion
In present study Grade 3 (44%) was most common followed by grade 2 (26%) followed by grade 4 (24%). In present study mean length of pterygium tissue was 2.52 mm with standard deviation of 1.06 mm, with the highest 4.5 mm and lowest 1 mm. There was positive correlation between grade of pterygium and KV – KH (diopter) and it was highly significant. It means as grade of pterygium increases, difference between KV-KH also increases (Spearman’s rho 0.482, p = 0.000). As, difference between KV-KH increases astigmatism increases compound hypermetropic astigmatism was seen in most of the cases of grade 3 and 4 pterygium, simple hypermetropic astigmatism was seen in grade 2 pterygium and Grade 1 pterygium causes only simple myopic astigmatism. After pteryguim surgery patients with grade 3 and grade 2 patients had drastic reduction in astigmatic error. Comparing pre-operative and post-operative refractive error after pterygium excision surgery shows that, in grade 1 pterygium simple myopic astigmatic error almost remains same. In Grade 2, 3 pterygium patients had no refractive error to mild simple myopic astigmatic error but compound hypermetropic astigmatism is completely nullified so patient with grade > 2 pterygium should undergo pterygium excision surgery. Similar study was carried out by Poonam Bhargava19 on 52 eyes of 50 patients with primary pterygium (32.69%) had grade III pterygium was seen in (32.69%), grade I (23.07%) and grade II (23.07%), grade IV was seen in 21.15%. Dr. Eknath Shelke20 found that out of 37 patients operated for pterygium with conjuctival autograft, 33 eyes belonged to Grade II and III pterygium (89.19%) only 2.70% had Grade I and 8.11% had Grade IV pterygium seen, which has a significant impact on vision. Maheshwari also got same results where 36 eyes had primary pterygium, where Grade II type of pterygium was most common i.e., 44.45% and Grade III pterygium was 33.33%. Similar observations were found in the study done by Fong8 and Avisar.21 Thus as the grade increases there is increase in astigmatic refractive error and hence the patient seeks for remedy.
In present study mean size of pterygium tissue was 2.52 mmwith standard deviation of 1.06 mm, with the highest 4.5 mm and lowest 1 mm. As the size of pterygium increases it makes the horizontal meridian flatter causing KH to increase there by increasing difference between keratometry readings (KV-KH) leading to increase in astigmatic refractive error. Lesions extending >45% of the corneal radius or within 3.2 mm of the visual axis produce increasing degrees of induced astigmatism.22 The authors reported that pterygium with larger than 2.2 mm extension might contribute to corneal astigmatism >2 D.23 Avisar A et al21 noted that as primary pterygium encroaches more than 1.00 mm size from limbus it causes with-the-rule significant astigmatism (> or = 1.0 diopter). Kampitak noted that pterygium induced corneal astigmatism and timing of pterygium excision surgery arevassociated with size of pterygium. He also noted that about 2 D of astigmatism is caused by 2.25mm of pterygium which should be considered as the limit of surgery.24
The present study shows that, mean spherical error (SE) (1.06 + 1.39) and astigmatic error (AE) (1.02 + 0.89) pre-operatively, on post operative day 1 and on regular follow up was statistically significant (p = 0.000). Spherical (0.08 + 0.23) and Astigmatic error (0.17 + 0.26) reduces significantly after pterygium excision surgery with conjunctival autograft with or without suture. Similar results were found in study done by Popat KB et al23 where Mean astigmatism preoperatively was found to be 6.20 ± 3.58 D which subsequently decreased to 1.20 ± 1.27 D on 45th post-operative day-showing 5.09 ± 3.32 D of change in astigmatism which was statistically significant (paired t-test, p<0.05). In the study done by Maheshwari S.25 corneal astigmatism reduced from 4.40±3.64 diopter (D) to 1.55±1.63D (P value <0.001) following surgery, which is comparable to our study. Also Stern and Lin reported improvement in topographic indices in 16 eyes ; they reported corneal astigmatism to reduce from (5.93–2.46D) to (1.92–1.68D).
The present study shows that with the rule astigmatism (58%) was most common pre-operatively followed by against the rule astigmatism (32%). Post-operatively, 68% subjects were having no astigmatism followed by against the rule astigmatism (14%). Similar results were found in study done by Eias Ali RT, Mohamed Ali AB on 100 Sudanese males and females aged between 18 and 45 years having pterygium in one eye and another eye being normal that The primary pterygium caused meridional steepness in corneal curvature (98%). With-the-rule corneal astigmatism was dominant (61%) (p<0.001). This result reveals that primary pterygium often leads to steepness in vertical meridian rather than horizontal meridian. This condition occurs because pterygium generally invade the cornea from the nasal side in a horizontal direction and this causes the horizontal meridian to flatten.26 Similar result was found by Avisar et al.24 Study carried out by Stern and Lin also suggested that pterygia induce asymmetric with-the-rule astigmatism.22
Present study shows, significant difference was seen in mean KV and KH pre-operatively, on post-operative day 1 after pterygium excision surgery with conjunctival autograft with or without suture and on regular follow up (p = 0.000), such that KV (43.84 + 1.01 decreases to 43.08 + 0.72) decreases while KH (41.30 + 0.96 increases to 42.56 + 0.79) increases following surgery and serial follow up. Similar results were seen by S. Maheshwari flattening was seen in the horizontal meridian, which was associated with astigmatism. It is thought to be caused by the formation of tear meniscus between the corneal apex and the elevated pterygium, causing an apparent flattening of the normal corneal curvature.27
The present study shows that, mean (KV minus KH) pre-operatively, on post operative day 1 and on regular follow up was statistically significant (p = 0.000). (KV minus KH) decreases (2.55 + 1.14 reduces to 0.60 + 0.41) after pterygium excision surgery with conjunctival autograft with or without suture, leading to reduction in refractive error i.e mean spherical error (SE) (1.06 + 1.39) and astigmatic error (AE) (1.02 + 0.89) pre-operatively reduced to Spherical (0.08 + 0.23) and Astigmatic error (0.17 + 0.26) post-operatively day 21. (p= 0.000) We found that Post-operatively, 56% subjects were having no refractive error followed by simple myopic astigmatism (26%). Post-operatively, 68% subjects were having no astigmatism followed by against the rule astigmatism (14%). Fong et al. in 1998 observed that pterygium excision usually induces a reversal of pterygium-related corneal flattening.8
In present study we found that simple myopic astigmatism (32%) was most common pre-operatively followed by compound hypermetropic astigmatism (28%). Post-operatively, 56% subjects were having no refractive error followed by simple myopic astigmatism 26%. With the rule astigmatism 58% was most common pre-operatively followed by against the rule astigmatism 32%. Post-operatively, 68% subjects were having no astigmatism followed by against the rule astigmatism 14%. In Grade 2, 3 pterygium patients had no refractive error to mild simple myopic astigmatic error but compound hypermetropic astigmatism is completely nullified. Other similar study done by Lin A, Stern GA. found that hypermetropic WTR astigmatism was but common.22 Pterygium results in high corneal astigmatism, which decreases following an excision.28 A pterygium-induced refractive change often leads to visual impairment, Keratometry measures only the central cornea and peripheral cornea is ignored and hence the results can be erroneous in eyes with pterygium.27 So, Computerized videokeratography remains the best tool in evaluating pterygium-associated corneal changes.27
In present study, the patient compliance On application of Mann-Whitney U test, pain score (done on basis of Wong Baker faces pain rating scale) after pterygium excision with conjunctival autograft without suture was lower than pain score in pterygium excision with conjunctival autograft with suture and difference between the two surgeries was statistically highly significant (p = 0.00).
There was no significant difference seen in post -operative after effects between two surgical techniques among patients ungergoing pterygium excision surgery. According to Dr. Mitra,29 “The main disadvantage of sutureless glue-free technique is the risk of graft loss in the immediate postoperative period.” In present there was 1 case of graft lost in sutureless technique and no such case in with suture technique. Foroutan et al.30 reported 20% of cases with graft retraction in his study. Suturing is more time consuming, lead to higher postoperative discomfort, higher recurrence, and complications than others, such as prolonged healing, fibrosis, and granuloma formation.31,32
In present study no significant difference was observed between mean vertical (KV) and horizontal (KH) corneal meridian or their difference (KV-KH) by two types of surgery (Pterygium excision with conjunctival autograft without suture or with suture) at various duration of study (p > 0.05). It mean in comparison between pre-operative and post-operative status there was equal reduction of KV, difference between KV & KH, increase in KH following two types of surgery. Though, till date, literature search reveals no similar study has been done we saw that as such there is no significant difference in keratometry readings and post operative refraction using these two different techniques, but patient discomfort (i.e. measured by pain score) is relatively less by using sutureless technique rather then doing pterygyium surgery with suture.
Conclusion
Pterygium leads to significant high corneal astigmatism, which hampers vision of the patient. Pterygium causes horizontal meridian flattening (KH). We concluded that, pterygium causes simple myopic with the rule type of astigmatism and compound hypermetropic astigmatism type of refractive error. There is drastic changes in keratometry readings pre-operatively and post surgical excision of pterygium tissue. Overall, after pterygium excision surgery most of the patients had no refractive error. After pterygium excision surgery compound astigmatic type of refractive error was nullified while there was no significant change in simple myopia. Post-operatively, spherical error was reduced and astigmatism was reduced to nullified. With the rule astigmatism was most common pre-operatively. Comparing pre-operative and post-operative refractive error after pterygium excision surgery shows that, in grade 1 pterygium simple myopic astigmatic error almost remains same. In Grade 2, 3 pterygium patients had no refractive error to mild simple myopic astigmatic error but compound hypermetropic astigmatism is completely nullified so patient with grade > 2 pterygium should undergo pterygium excision surgery. We concluded, that with increase in the size of pterygium amount of cornea induced astigmatism also increases. There is definite change in refractive status in pterygiyum post pterygium surgery so with this study I would like to deduce that, to get emmetropic status for cataract surgery or refractive cataract surgery.