Author Details :
Volume : 5, Issue : 1, Year : 2019
Article Page : 28-30
https://doi.org/10.18231/2581-5016.2019.0007
Abstract
Purpose: To evaluate the outcome of nasolacrimal duct probing in children older than two years in congenital nasolacrimal duct obstruction.
Materials and Methods: A Hospital based prospective interventional study of 20 cases of congenital nasolacrimal duct obstruction above 2 years of age was done. A thorough preoperative evaluation was done and diagnosis confirmed by negative Fluorescein dye disappearance. Patients underwent probing under general anaesthesia. Cases were followed up at 1, 4 and 12 weeks postoperatively. Successful outcome was assessed in terms of absence of watering or discharge and also positive Fluorescein dye disappearance test done at each follow up visit. Data was collected and analysed using descriptive statistics.
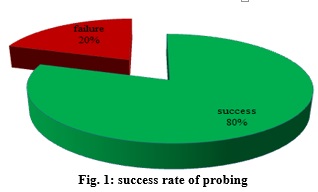
Results: 23 eyes of 20 patients of simple congenital nasolacrimal duct obstruction in the age group of 2-6 years were included in our study. Lacrimal sac massaging was done previously in 17(85%) cases. 3(15%) patients underwent bilateral probing and 17(85%) unilateral probing. 16(80%) out of 20 patients had successful outcome in terms of resolved symptoms and signs.
Conclusion: Late probing can be done as a primary intervention in children above 2 years of age with successful outcome instead of going directly for major procedures like dacrocystorhinostomy.
Keywords: Congenital nasolacrimal duct obstruction, Probing, Flourescein dye disappearance test, Sac massage, Epiphora.
Congenital nasolacrimal duct obstruction (CNLDO) is the most common cause of epiphora in newborn children.[1]This condition results from failure of canalization of the nasolacrimal duct. The obstruction is most commonly at the valve of hasner where the nasolacrimal duct opens into inferior meatus of the nasal cavity. This may occur either due to persistence of a membrane at the distal end of the duct, bony obstruction or narrowing of the inferior meatus with apposition of the nasal mucosa. Prevalence of the disease varies from 0.5% to 20% according to various studies.[2],[3]Complications of the condition include recurrent conjunctivitis, acute and chronic dacrocystitis and dacrocystocele. It is noted that about 30% of full term infants have obstruction at birth.[4]But spontaneous resolution occurs in upto 96% of the cases.
Management of CNLDO initially includes Crigler technique of sac massage which aims to open up any membranous obstruction at the lower end of the duct by increasing the hydrostatic pressure.[5]When this fails to relieve epiphora, probing is indicated. This is currently the standard surgical management of CNLDO and relieves the obstruction using an appropriately sized Bowman’s probe. However optimal timing of probing remains controversial. Few studies have shown that success of the surgery decreases as the age advances, while other studies demonstrate the success of the procedure not only depends on age of probing but also on the type of obstruction. This study was conducted to evaluate the outcome of probing in cases of simple CNLDO in children more than 2 years of age.
This is a hospital based prospective interventional study conducted in our hospital from January 2017 to September 2018. Patients with complaints of watering or discharge were evaluated for epiphora at our pediatric ophthalmology clinic. The study was undertaken after obtaining clearance from ethical committee and institutional review board. Informed consent was taken from parents. Children aged 2 years and above with complaints of watering from or within 4weeks of birth were included in the study. Exclusion criteria were previous surgical history of probing, trauma to maxilla- facial region, nasal pathology, cranio- facial abnormalities and local lid pathology. Ophthalmic evaluation included slit lamp examination to rule out local ocular causes of watering, routine fundoscopy, cycloplegic refraction to look for co- existing refractive errors and Fluorescein dye disappearance test. After confirming the diagnosis, cases were admitted and posted for probing under general anaesthesia. Paediatrician and Anaesthetist clearance was obtained for all patients to undergo the procedure under general anaesthesia.
The eye /eyes to be operated was painted and draped under sterile conditions. The probing was performed through upper punctum in all our patients. Under general anaesthesia, dilatation of the upper punctum was done with Nettleship punctum dilator. Probing was carried out using an appropriately sized Bowman’s lacrimal probe. The probe was introduced vertically into the punctum and then rotated horizontally in the same plane to enter the canaliculus and then advanced until it reached the nasal wall of thelacrimal sac fossa, giving the sensation of a hard stop. The probe was then gently retracted and turned downwards by 90 degrees and advanced further in a downward, and backward direction to approach the lower end of the nasolacrimal duct. A sudden give away feel was appreciated due to the opening up of membranous obstruction at the lower end of nasolacrimal duct. In all our patients, we appreciated hard stop, ruling out canalicular obstruction. The entire passage of the probe was a single and smooth one so that there is no creation of false passage and also ruled out complex obstruction. Antibiotic eye drop was instilled at the conclusion of the procedure. Patients were discharged the following day. Postoperative treatment included Dexamethasone 0.1% with Moxifloxacin 0.5% eye drops 8times a day tapered weekly for one month and saline nasal drops 3 times a day for 3 days. The patients were followed up at 1 week, and 4 weeks and 3 months postoperatively. Successful outcome was considered as complete remission of watering and discharge after the procedure and also clinically by flourescein dye disappearance test. Data was collected and analysed using descriptive statistics.
Results
23 eyes of 20 patients of simple CNLDO in the age group of 2 to 6 years were included in our study. 18 (90%) were males and 2(10%) females with mean age of 3.2 years (Table 1). Right eye was involved in 8(40%) cases, left eye in 9(45%) and bilateral in 3 (15%) cases (table 2). Conservative treatment in the form of lacrimal sac massaging had been done previously in 17(85%) cases. 3(15%) patients underwent bilateral probing and 17(85%) unilateral probing. 16(80%) out of 20 patients had successful outcome in terms of resolved symptoms of watering/discharge and positive flourescein dye disappearance. 4 (20%) cases had persistent watering and were planned for dacryocystorhinostomy later.
Table 1: Age distribution
|
Age (years) |
Frequency (%) |
|
2-3 |
7(35%) |
|
3-4 |
7(35%) |
|
> 4 |
6(30%) |
Table 2: Laterality
|
Laterality |
Frequency (%) |
|
Right |
8(40%) |
|
Left |
9(45%) |
|
Bilateral |
3(15%) |
 |
Click here to view |
Probing is the standard procedure of choice for cases of CNLDO where conservative treatment like lacrimal sac massage has not been successful.[6],[7]However timing of the surgery and success of the procedure with respect to age remains controversial with some studies showing reduced success of the procedure with increasing age.
In a study done by Ugarbas et al, showed that the cure rates were 92% in the first year, 84.5% in the second year, 65% in the third year, and 63.5% inthe fourth and fifth years of age.[8] Katowitz and Welsh reported success rate of 97% in initial probing in children less than 13 months and 54.7% above 13 months of age.[9] Mannor GE et al, in their study, documented cure rate of 92% in less than 1 year of age and progressively reduced rates of 42% at 60 months of age.[10] Eshragi B[11] demonstrated success rate of more than 50% in children between 24-35 months, 66.7% in patients aged 36-47 months and 44.4% between 48-60 months. In his study, Honavar et al (2000) demonstrated that age more than 36 months, bilateral obstruction, a dilated lacrimal sac, non-membranous obstructions and failure of earlier probing decreased the success of the procedure.[12]
In our study, we included children in the age group of 2-6 years. 85% of the cases had undergone conservative management like lacrimal sac massaging previously following which they didn’t have resolution of watering of eyes. This could be because of ignorance of importance of massaging, illiteracy, improper technique of massage and lack of compliance and follow up. 80% of patients who underwent probing had successful outcome. 20% of the cases had persistent watering, who were planned for dacryocystorhinostomy at the later date.
Our study showed considerably good results of probing in older children for congenital nasolacrimal duct obstruction. Study done by Maheshwari showed success rates of 80.95% in children aged 2–7 years with non complicated obstruction.[13] Guler et al showed successful results of 90% in children up to 9years of age.[14] Table 3 shows the success rate of probing in older children in various studies in comparison to our study results.
In our study, we documented success rate of 80% between 24 to 60 months of age. However, we cannot comment about success rate in complex obstruction since we didn’t encounter them in our cases and further study is needed to analyse the outcome of probing in them.
We conclude that nasolacrimal duct probing under general anesthesia is a worthwhile option for the treatment of simple CNLDO for children who present later than 24 months of age before undertaking major procedures like Dacrocystorhinostomy.
Conflict of Interest: None.
How to cite : Shwetha H. R, Kulkarni V M, Study of outcome of late probing in congenital nasolacrimal duct obstruction. IP Int J Ocul Oncol Oculoplasty 2019;5(1):28-30
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 1611
PDF Downloaded: 517