Author Details :
Volume : 5, Issue : 1, Year : 2019
Article Page : 24-27
https://doi.org/10.18231/2581-5016.2019.0006
Abstract
Introduction: This study is done to assess the efficacy of powered endoscopic dacryocystorhinostomy (DCR) with large bony ostium exposing of fundus of sac and primary mucosal anastomosis. The study involved prospective interventional case series with short perioperative follow up.
Materials and Methods: Operative and postoperative data were prospectively collected on 42 patients (15 men and 27women; mean age, 62.4 y; range 14–91 y) who presented to a lacrimal clinic with epiphora and obstruction of the nasolacrimal system and who consecutively underwent either primary or revision powered endoscopic DCR. All surgeries done by the same surgeon by standardized surgical technique. Follow?up evaluations included symptom evaluation and endoscopic assessment of the newly created ostium with fluorescein testing at each postoperative visit.
Results: The only surgical complication was one case of sub cutaneous emphysema. 39 of the 42 DCRs had anatomically patent naso lacrimal duct after a mean follow?up of 12 months (standard deviation = 5 months), yielding a success rate of 95.7%. Out of three failures two had closed ostium because of improper use of medications, one patient had granulation tissue at the ostium. Two patients with a patent ostium had functional block and continued to have some symptoms.
Conclusion: Powered endoscopic DCR which meets the with full sac exposure and primary mucosal apposition has a success rate comparable to that achieved with external DCR.
Keywords: Endonasal DCR, Powered DCR, Dacryocystorhinostomy.
Dacryocystorhinostomy (DCR) is surgical procedure done for epiphora due to nasolacrimal duct obstruction (NLDO), which involves creating a fistulous opening between lacrimal sac and nasal cavity at the level of middle meatus. There are various procedures to create this ostium that is external DCR, endoscopic nasal DCR, laser DCR. The most accepted are external and endonasal DCR. Endonasal DCR initially had guarded acceptance because of inconsistent success rates. External DCR which is considered to be the gold standard procedure, now because of the introduction of newer techniques even endonasal DCR has success rate as comparable to the external DCR.
In The conventional endonasal DCR the main hurdles are removing the thick maxillary process and creating a large ostium to expose the fundus of the lacrimal sac. The use of powered instruments to debride the thick bone has increased the success rate of endonasal DCR.
In this study our objective is to evaluate the effectiveness of powered endonasal DCR that is removal of medial wall of the lacrimal sac with powered instruments Marathon M4 lab micro motor burr, which is economically most affordable compared to other micro motor burrs and preservation of the mucosa. In this study we have included 42 patients with NLDO who have undergone powered endonasal DCR by the same surgeon. The outcome and long term patency of the ostium were evaluated.
Inclusion criteria
Patients with nasolacrimal duct obstruction
Patients above the age of 12 years
Failed DCR
Canalicular obstruction
Primary nasal pathology (severe atrophic rhinitis, nasal polyp, gross DNS)
42 patients with complain of watering coming to lacrimal clinic between 2016 February to 2017 April were included in our study. Among them 15 were males and 27 were females. The most common aetiology of presentation was Primary Acquired naso lacrimal Duct Obstruction (PANDO), (Table 1). All the patients underwent thorough ocular examination, sac syringing, endoscopic examination of nasal cavity pre operatively (table 2) and patients with above inclusion criteria were included in the study.
Surgical technique
All the cases done under local anesthesia using 45 degree 4mm nasal endoscope. Nerve blocks are given to supratroclear nerve at supraorbital notch, ethmoidal nerve block is given at medial canthus, infraorbital nerve block given at infraorbital notch using 2%lignocain and 1:100000 adrenaline mixture. Nasal pack with 4% lignocaine and 2 ampules of adrenaline mixture placed for 20 minutes before surgery. Nasal mucosal infiltrate at the lateral nasal wall near middle meatus, middle turbinate and medial nasal wall is given using the same 2% lignocaine and 1:100000 adrenaline mixture.
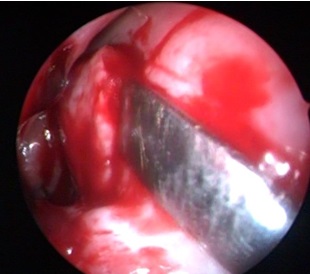
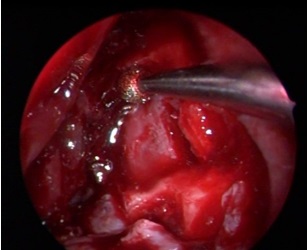
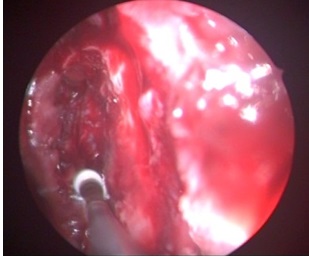
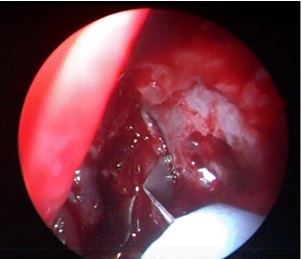
An inferior based mucosal flap is created with crescent (Fig. 1) blade first incision starting 10mm above the middle turbinate extending down till inferior turbinate, second vertical incision of similar length taken 10mm in front of the first incision, then these two vertical incisions are joined together at the superior margin using 15 no surgical blade. This mucosal flap is then reflected (Fig. 2) on the inferior turbinate. The bone seen now is the frontal process of maxillary bone. The bone punch is begun with Kerrison’s bone punch. Since the bones in the nasal cavity are placed sagittaly bone punch becomes difficult as we go up then theses burrs come to our rescue. With the help of these cutting and diamond burrs (Fig. 3,4) the thickness of the bone is reduced which provides good bone grip, enlarges the ostium exposing the fundus of the lacrimal sac and smoothens the bony margin to prevent granulation tissue formation.
When the sac is exposed till the fundus canaliculi are intubated with bowman probe tenting the sac in the nasal cavity. The sac is cut opened vertically with the help of keratome (Fig. 5) then two horizontal incisions are given with sickle knife creating two anterior and posterior flaps. This marsupialises the lacrimal sac into the nasal cavity. Then the inferior based flap is reflected back on the bare bone.
Light nasal packing is done with antibiotic ointment which is removed after 24 h. The patients were discharged on the next day with antibiotic coverage and saline nasal sprays. Lacrimal syringing was done on the first day, 1week, 1month post-operative following which they were followed-up twice monthly for minimum of 8 months. At each follow-up visit, lacrimal syringing with nasal endoscopy was done to visualise the patent ostium.
Results
Operative and postoperative data were analysed on 42 patients (15 men and 27women; mean age, 62.4 y; range 14–91 y) who presented to a lacrimal clinic with epiphora and obstruction of the nasolacrimal system and who consecutively underwent either primary or revision powered endoscopic DCR.
Among 42 patients pre op endoscopic examination showed 5 patients with mild deviated nasal septum, 2 with hypertrophied inferior turbinate and 3 patients with mild atrophic rhinitis which was treated before surgery (table 2). Intra operatively 2 patients had posteriorly placed lacrimal sac. Post-operative endoscopic examination 3 patients had granuloma near the ostium among which 1 was covering the ostium leading to surgical failure,2 patients had closed ostium because of improper use of medication and 2 had functional block with FDDT.
The surgical complications were two case of sub cutaneous emphysema which resolved in two weeks, one patient had post nasal bleed following surgery with increased blood pressure. 39 of the 42 patients had anatomically patent ostium after a mean follow-up of 12 months (standard deviation = 5 months), yielding a success rate of 95.7%.
Table 1: Etiology of presentation
|
Aetiology of presentation |
Number of patients |
|
Primary acquired nasal duct obstruction (PANDO) Failed DCR Acute dacryocystitis |
33 5 3 |
Table 2: Endoscopic examination findings Pre, Intra and post surgery
|
Endoscopic examination |
Number of patients |
|
Pre-operative Mild deviated nasal septum Inferior turbinate hypertrophy Mild atrophic rhinitis |
5 2 3 |
|
Intra operative Posteriorly place lacrimal sac |
2 |
|
Post-operative Granulation tissue Closed ostium Functional block |
3 2 2 |
 |
Click here to view |
Fig. 1 Mucosal incision with crescent blade
 |
Click here to view |
Fig. 2 Inferior based mucosal flap reflection
 |
Click here to view |
Fig. 3 Enlarging the ostium superiorly with diamond burr
 |
Click here to view |
Fig. 4 Enlarging the ostium inferiorly with cutting burr
 |
Click here to view |
Dacryocystorhinostomy is surgery of choice for NLDO. In endonasal DCR important factors that determine the long-term patency are creating a large ostium and mucosal apposition which helps in healing by primary intention and prevent granulation tissue formation.[1] The importance of mucosal flap preservation is still under debate.[2]
In our technic use of diamond burr increases the success rate of endonasal DCR. Utilization of diamond burr helps to make a large ostium. Drilling the bone helps to reduce bone thickness and provide a good grip of the bone to punch it. It smoothens the bony margin of the ostium to reduce the granulation tissue formation
Neil C Tan et al., in their study, concluded that surgical outcome depends on the ostium size and that significant shrinkage of the DCR ostium occurs in the first 4 weeks post-operatively.[3] Hence, it is not just the creation of a wide sac ostium which is important; the first few weeks of healing also plays a big role in determining long term patency.
P J Wormald (2012) in his study said that adequate exposure of the lacrimal sac requires exposure above the level of the axilla of middle turbinate using a drill. This was found to be important to ensure success of the procedure.[4]hence these powered instruments help to remove thick bone and expose the fundus of the lacrimal sac.
Endoscopic DCR has many advantages as compared to external DCR—avoidance of facial scaring, non-division of medical canthal ligament, performed as a day care procedure, limited tissue damage and preservation of the pump action of the lacrimal sac of the orbicularis oculi muscle.[5],[6]
Wormald PJ et al Studied Operative and postoperative data in 47 patients and Concluded that Powered endoscopic DCR with full sac exposure and primary mucosal apposition has a success rate comparable to that achieved with external DCR.[7]
Ali MJ et al done A retrospective review of 283 patients and concluded that Powered endoscopic DCR is a safe procedure and offers excellent results both in primary and revision DCRs. The threshold to perform adjunctive endonasal procedures should be very low when indicated.[8]
The overall success rate (95.7 %) of our new technique is comparable to the previous studies and further validation of this new method requires larger randomised control trials. These economically affordable instruments can be owned by all endoscopic DCR surgeons to have a high success rate.
Conclusion
Powered endoscopic DCR which meets the with full sac exposure and primary mucosal apposition has a success rate comparable to that achieved with external DCR.
Conflict Of Interest: None.
How to cite : Kulkarni S, Satyamurthy K V, Hiremath R, Jain A, Powered endoscopic dacryocystorhinostomy (DCR), raising the bars. IP Int J Ocul Oncol Oculoplasty 2019;5(1):24-27
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 1771
PDF Downloaded: 502