Author Details :
Volume : 5, Issue : 1, Year : 2019
Article Page : 15-20
https://doi.org/10.18231/2581-5016.2019.0004
Abstract
Aims and Objectives: Ocular burns consist of burns to the sclera, conjunctiva, cornea, and eyelids. Among the etiologic agent’s thermal injuries are caused by Radiant energy (heat, electricity) and Ultraviolet [UV] radiation. For thermal burns, severity is determined by the dept & degree of epithelial damage and limbal ischemia. Severe collagen shrinkage leading to severe excavating corneal ulcer occurs due to coagulative necrosis. So early active management (medical and surgical) is required for restoration of maximum possible vision and provide maximum cosmesis to the patients.
Methods: Our study is a prospective, observational and interventional study of 3 case series who presented to the Emergency Department (ED) following cracker injury with three different clinical scenario. In our study we considered 3 patients presenting with ocular thermal burn (cracker burn) in the emergency department with three different clinical pictures. Active management was done in these patients in initial days and then were considered for Amniotic Membrane Grafting (AMG), Penetrating Keratoplasty (PK) in 2 patients respectively and Epithelial Stripping in the third patient. They were subsequently followed up for 6 months and the prognosis was noted in terms of vision and cosmetic aspects.
Conclusion: Early active management whether medical or surgical, in thermal burn cases can provide early mobility and better cosmesis to the patients with almost full recovery of vision
Keywords: Thermal ocular injury, Ocular burn, Amniotic membrane transplantation, Penetrating keratoplasty, Epithelial stripping.
Introduction
Chemical or Thermal ocular burns represent about 10% of ocular traumas.[1] According to USA statistics ocular burns represent 7-18% of the eye injuries seen in Emergency Departments.[2] Thermal burns account for 16% of ocular burn cases.[3] Approximately 15-20% of patients with facial burns exhibit ocular injury.[4] In India two studies conducted in Ashwini Rural Medical College and Research Centre, Solapur and R.P. centre AIIMS Delhi showed incidence to be 5% and 10% respectively.[5][6] Thermal injuries are potentially blinding eye injuries and constitute true emergencies but are less common than chemical injuries with very different form of ocular insult, post injury problems and treatment approaches. Work-related, domestic or recreation accidents, as well as assaults are the main sources of ocular burns. Cell death from thermal burns is limited to the superficial epithelium; however, thermal necrosis and penetration can occur due to severe coagulative necrosis. With UV burns, epithelial injury results in a punctate keratitis. Although the pain is often delayed, UV corneal burns are exquisitely painful.[7] Thermal injuries can be caused by hot substances (e.g. cracker, fire, irons, hot curlers, cigarettes, and hot liquids). Hot liquids have been known to splash into the eye from substances that explode after removal from a microwave; steam from hot liquids is also a potential cause. Fire is a common cause of burns to the face and eyes. Welders who view the arc without protective goggles are at risk for injury. Lasers used in industry, military, and medical practice also can cause ocular burns.[8]
Our study was a prospective, observational and interventional study with 3 cases of Ocular Thermal Burns who presented to us with three different clinical scenarios. The mode of burn was cracker injury in all the 3 cases as the study was conducted during festive season (Diwali). All the cases were managed conservatively in the acute stages. Three different surgical intervention were carried out in all 3 cases depending on the severity and area of concern with aim to attain maximum possible vision and cosmesis was in all the cases.
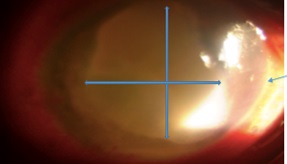
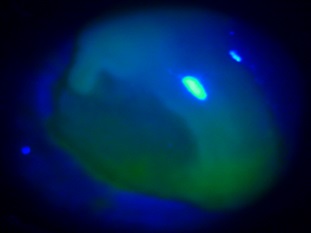
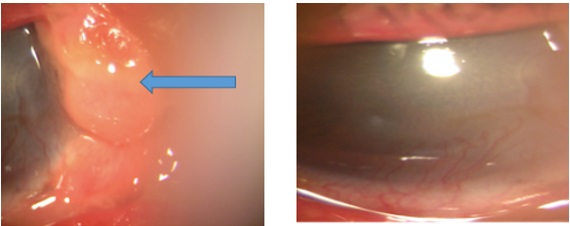
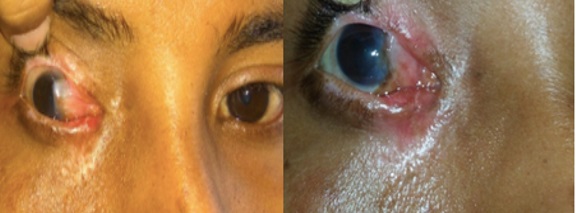
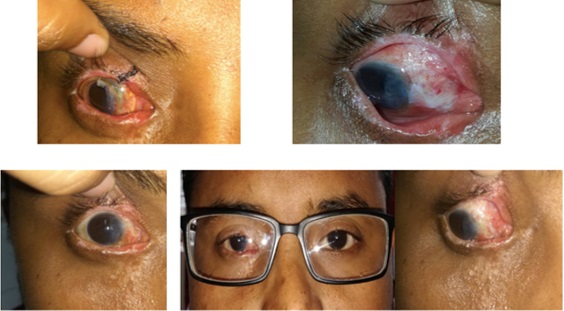
Case no. 1: 27 year old male came to emergency at midnight with sudden onset painful DOV unable to open Right Eye, photophobia, watering and burn over right side of face following cracker burn (Fig 1). General examination was within normal limit. Vision in R/E was FC at ½ metre and 6/6 in Left Eye(L/E). R/E findings: EYELIDS: superficial burn over eyelids involving cheek, nose, forehead, eyebrow and grossly swollen eyelids with eyelashes burnt. CONJUNCTIVA: chemosed, congested, carbon particles embedded CORNEA: Epithelial defect (9 X 7.5 SQ.MM) (positive fluorescin) inferior and nasal half; deep stromal edema, limbal ischemia(less than 1/3rd) noted nasally (ROPER HALL CATEGORY II Limbal ischaemia) ANTERIOR CHAMBER: 0.5mm exudative debris deposits (Fig 2,3) IRIS: periphery iris details appeared normal. Rest ant. segment: details could not be elicited. LE showed few superficial skin burn. Initial management was started with thorough saline wash and burnt necrotic tissues and carbon particles were debrided with utmost care. Topical antibiotic (e/d and e/oint Moxifloxacin), topical cycloplegic, artificial tear substitute frequently (gel) systemic antibiotic and analgesics. Plastic surgery opinion was taken for the skin burn. On 10th day vision in RE improved to FC 3M, blepharospasm reduced. Cornea showed epithelisation and leucomatous opacity of 4x3 sq. mm, superficial and deep vascularisation noted inferiorly, edema was partially reduced. (Fig. 4). Patient was started on topical prednisolone 2hourly. Patient was discharged on 15th day with medications as followed: E/d Prednisolone 6 times with tapering on 7th day, E/d Topin1%, Tear Substitute every 2-3 hourly, E/oint. D-Panthenol once at bedtime. Vision on 15th day improved to 6/60. At 1-month follow-up although vision improved to 6/36, Eyelid granuloma was noted superonasally and Symblepheron behind the granuloma. (Fig, 5,6) Granuloma excision with Symblepheron release was done RE. At 2 month follow-up: Vision in RE was 6/36, Granuloma excision site showed lid coloboma and Recurrent Symblepheron noted superonasally with Pseudopterygium. (Fig. 7, 8) Pseudopterygium excision and Symblepheron release with Amniotic Membrane Grafting was done and Lid coloboma was repaired using 6-0 nylon.Symblepheron ring was put in situ for 2 weeks (Fig. 9,10). At 6-month follow-up the patient came with a Vision in RE 6/12 (BCVA), Corneal edema was almost clear with opacity (MACULAR GRADE) nasally, Amniotic membrane in-situ. (Fig. 11,12,13).
 |
Click here to view |
Fig. 1: superficial skin burn over eyelids, forehead
 |
Click here to view |
Fig. 2: stromal edema with limbal ischaemia involving 3 clock hours and exudative debris in AC
 |
Click here to view |
Fig. 3: epithelial defect in cobalt blue light
 |
Click here to view |
Fig. 4: on 10th day leucomatous opacity with stromal edema and inferior vascularisation (superficial and deep)
 |
Click here to view |
Fig. 5,6: at 1 month follow-up eyelid granuloma and symblepharon in superonasal quadrant
 |
Click here to view |
Fig. 7,8: 2 month follow-up following granuloma excision and symblepheron release showed recurrent symblepharon and pseudopterygium formation. Skin burns almost healed with no contracture
 |
Click here to view |
Fig 9: Figure showing Amniotic membrane in situ in R/E, fig 10: showing lid coloboma repaired with 6-0 nylon and symblepharon ring kept in-situ., Fig 11,12,13: showing final picture at 6 month showing clear cornea with macular opacity nasally, AMG in-situ and BCVA 6/12
 |
Click here to view |
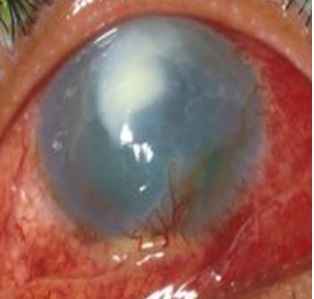
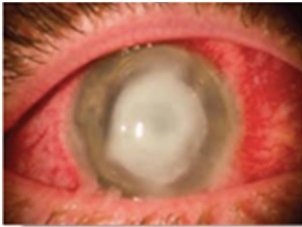
Fig. 14: Case number 2 presented after 1month with central corneal apacity and congestion in LE following cracker burn
 |
Click here to view |
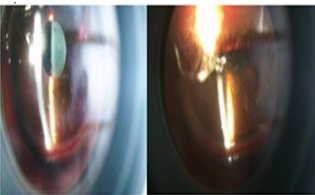
Fig. 15: 1st post op: mild graft edema with air bubble in anterior chamber, stitches in-situ.
 |
Click here to view |
Fig. 16: at 9 month follow up post PK, graft was clear with ant segment details within normal Limits
 |
Click here to view |
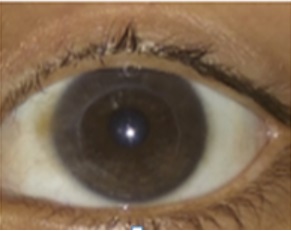
Fig. 17: 9Years old boys with periocular, facial and ocilar involvement following cracker burn
 |
Click here to view |
Fig. 18-19: embedded cabon Particles in epithelium and superficial stroma of cornea.
 |
Click here to view |
Fig 20: at 3 weeks post op patient was comfortable with vision 6/6 OU.
Thermal ocular burns being one of the urgent ophthalmic emergencies, often resulting in permanent damage, and in some cases, blindness need active management. In our case series we have shown the role of Amniotic Membrane Graft(AMG), Penetrating Keratoplasty without Limbal stem cell Graft and Total Epithelial Stripping of cornea in attaining good visual outcome and full cosmesis in 3 different scenario of thermal ocular burn. Studies have reported successful treatment of mild-moderate ocular burns using AMG with or without limbal cell transplantation.[9],[10],[11],[12],[13] In cases of severe burns, AMG restored the conjunctival surface but did not prevent limbal stem cell deficiency, which required further limbal stem cell transplantation.[12],[13]Kobayashi et al reported 5 eyes of 5 pts and concluded that immediate AMG is quite useful for managing moderately severe acute thermal injury by facilitating rapid epithelisation and pain relief and securing ocular surface integrity.[14] Although no relevant information on role of Total corneal epithelial stripping was found, our case showed significant improvement and attained 6/6 vision at 4 weeks’ time. Julias T.S Theng and Yu-Feng et al[15] in their individual studies showed the role of combined Autologous Limbal Grafting and Penetrating Keratoplasty for severe corneal burns following corneal burns. Roper-Hall graded ocular burn according to quadrant of limbal ischemia and severity of corneal involvement.[16]However, in the years following the introduction of the Roper-Hall classification, the knowledge and understanding of ocular surface healing and approach to surgical management of ocular surface burns has changed dramatically. The understanding and clinical application of the concept of limbal stem cells of the corneal epithelium and forniceal stem cells of the conjunctival epithelium, has significantly improved the outcome of treatment in patients with ocular surface burns.[17],[18],[19]Taking all these factors into account Harminder S. Dua et al modified the Roper-Hall classification and graded ocular burn according to clock hour involvement of Limbal area rather than Limbal Ischaemia which included Limbal epithelial defect with or without limbal ischaemia.[20] The best outcome is to be expected when a “burn injury” produces a corneal epithelial defect without any limbal or conjunctival involvement. In our study case no 3 had the best outcome among all three. Dua et al mentioned in their study that when less than 3 clock hours of the limbus are involved and less than 30% of the adjoining or adjacent conjunctiva is also involved, a good prognosis can be expected with conventional medical management.[21]This includes measures such as copious irrigation soon after injury, use of topical vitamin C drops, citrate drops, acetylcysteine drops, judicious use of steroids, and prophylactic antibiotics.[22] A good outcome can also be expected when limbal involvement is between 3 and 6 clock hours associated with conjunctival involvement of between 30% and 50%. Ballen first suggested a classification which was later modified by Roper-Hall to provide prognostic guidelines based on the corneal appearance and the extent of limbal ischaemia.[23] In our first case although the limbal involvement was <3>
Conclusion
Fire-cracker injury is the most common cause of ocular thermal burn in India mostly affecting young males. Thermal burns result from accidents associated with firework explosions, steam, boiling water, or molten metal (commonly aluminium) Historically, it has been recognised that the extent of tissue damage is a prognostic indicator of recovery following ocular surface injury. Recovery of ocular surface burns depends upon the causative agent and the extent of damage to corneal, limbal, and conjunctival tissues at the time of injury. Damage to intraocular structures influences the final visual outcome. Besides conventional medical management as mentioned above, it is important to monitor these patients closely with regard to conjunctival epithelial migration on to the corneal surface
Conflict of Interest: None.
How to cite : Kalita I R, Singh H V, Ocular thermal injury: Study on its management considerations, visual outcome and cosmesis in tertiary health care system. IP Int J Ocul Oncol Oculoplasty 2019;5(1):15-20
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 5471
PDF Downloaded: 663