Author Details :
Volume : 5, Issue : 1, Year : 2019
Article Page : 12-14
https://doi.org/10.18231/2581-5016.2019.0003
Abstract
Introduction: Occlusion of the lacrimal duct will cause inflammation and accumulation of the harmful materials and pathogens, in the conjunctival sac, raising the risk of corneal infection.7 Hence this study was conducted to investigate the prevalence of lacrimal duct obstruction in patients suffering from fungal keratitis.
Materials and Methods: This was a prospective study conducted for a period of one year from July 2017 to July 2018. Forty fungal keratitis cases were studied. Detailed personal history along with presenting symptoms was collected. Patency of lacrimal duct was confirmed by lacrimal syringing. Ocular investigations and microbiological investigations were done standard techniques. Data collected was tabulated and results obtained were analyzed by counts and percentages using MS Excel, 2007 version.
Results: Out of 40 cases, 29(72.5%) cases were male and 11(27.5%) cases were female. Two cases (5.0%) had nasolacrimal duct obstruction. Both were male patients aged 57 years and 65 years respectively. First male patient had right eye involvement and the second male patient had left eye involvement.
Conclusion: Out of 40 cases of fungal corneal ulcer, 2 cases (5.0%) had nasolacrimal duct obstruction. Though the incidence of fungal corneal ulcer with concurrent nasolacrimal duct obstruction is low, a thorough evaluation of lacrimal apparatus has to be performed.
Keywords: Fungal corneal ulcer, Chronic Dacrocystitis, Nasolacrimal duct obstruction.
Corneal diseases are a major cause of vision loss and blindness, and caused by bacteria, fungi and protozoa. However, with in the tropics, as many as two third of ulcers may be due to filamentous fungi and distribution may vary considerably between continents and countries and also within countries.[1]According to the World Health Organization, corneal diseases are a major cause of vision loss and blindness, second only to cataract in overall importance.[2]The typical feature of fungal infection is slow onset and gradual progression, where signs are much more than the symptoms. Keratitis due to filamentous fungi is believed to usually occur following trauma, the key predisposing factor, in healthy young males engaged in agricultural or other outdoor work.[3]
In India the common fungi isolated are Fusarium species, Aspergillus species and rarely, pigmented fungi.[4]While some of the clinical features of fungal keratitis are suggestive of fungal infection, none of them can be considered absolutely pathognomonic of a particular type of etiological agent.[5]
Numerous studies on how to control and to treat fungal corneal ulcers have been reported previously, the relationship between fungal keratitis and the disorders of neighboring tissues/organs such as chronic dacryocystitis, has not been systematically explored previously.[6]Lacrimal apparatus consists of upper and lower puncta, canaliculi, common canalicular duct, sac, nasolacrimal duct draining tear film from the surface into the nose.[6],[7] Occlusion of the lacrimal duct will eventually cause inflammation and accumulation of the harmful materials and pathogens, in the conjunctival sac, raising the risk of corneal infection dramatically.[8] Hence this study was conducted to investigate the prevalence of lacrimal duct obstruction in patients suffering from fungal keratitis.
This was a prospective study conducted at a tertiary care hospital in North Karnataka region for the period of one year from July 2017 to July 2018. Forty patients suffering from fungal keratitis were included in this study. Detailed history of personal details along with presenting symptoms was collected. Significant past history and treatment history were noted. Detailed ocular examination was done. Ocular investigations included lacrimal sac syringing and flourescein staining. Lacrimal patency was checked by lacrimal syringing. Lacrimal syringing was performed by instilling a drop of 4% lignocaine into the conjunctival sac. The lower punctum was dilated with a punctum dilator. A 5ml syringe filled with distilled water attached to a lacrimal cannula was inserted into the lower canaliculus and lacrimal passage was irrigated. Nasolacrimal duct obstruction was diagnosed by regurgitation of fluid into the conjunctival sac by applying pressure over the lacrimal sac area. Flourescent staining was performed using 2% Flourescein stain. Corneal scrapings were collected using sterile Bard-parker blade under strict aseptic conditions. Microbiological investigations were done for corneal scrapings to rule out the etiology. Gram’s stain, KOH mount, bacterial culture and fungal culture were performed using standard microbiological techniques. A 10% KOH mount was performed for corneal scrapings and observed under 40X magnification for fungal elements. The corneal scrapings were also inoculated onto Blood Agar and Sabourauds Dextrose Agar for aerobic bacterial and fungal cultures respectively.[9] Blood Agar was incubated for 48 hours at 370C and Sabourauds Dextrose Agar was incubated in BOD incubator at 220C for 14 days. Fungal culture plates were observed for fungal growth for up to two weeks. Identification of fungal growth was done by macroscopic examination of colony morphology, pigment production and microscopic examination by lactophenol cotton blue preparation. Data collected was tabulated and results obtained were analyzed by counts and percentages using MS Excel, 2007 version. Ethical clearance for this study was obtained from the institutional ethical committee.
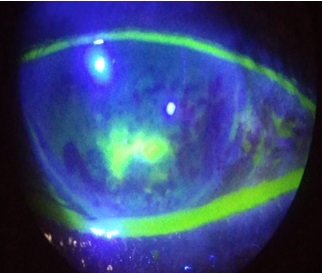
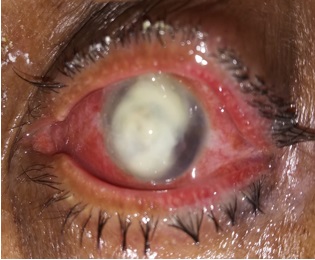
Total of 40 cases of fungal corneal ulcer were studied for a period of one year, out of which, 29(72.5%) cases were male and 11(27.5%) cases were female. Significant history of watering of eye was given by 10 patients (25%), while the remaining 30 patients (75%) did not complain of epiphora. Trauma history was given by 33 patients (82.5%) and no other predisposing factor was found in the study patients like dry eyes, steroid use or any lid disorders. Out of 40 cases of fungal corneal ulcer, 38 cases (95%) had patent nasolacrimal duct and only 2 cases (5.0%) had nasolacrimal duct obstruction. Both the cases were rural dwelling male patients aged 57 years and 65 years respectively. First male patient had right eye involvement and the second male patient had left eye involvement. All the 40 cases (100%) were KOH mount positive for fungal elements but only 9 cases (22.5%) were positive for fungal growth. Out of the 9 cases, 5(55.55%) displayed isolation of Fusarium species, 2(22.22%) showed Penicillium species, 1(11.11%) case showed Aspergillus and 1(11.11%) case showed growth of Curvularia which is a dematacious fungus. The two fungal corneal ulcer patients with nasolacrimal duct obstruction were both fungal culture negative. The two cases with nasolacrimal duct obstruction are described in detail under Image 1 and Image 2 respectively.
 |
Click here to view |
Fig. 1: Case 1: Patient with partial nasolacrimal duct obstruction, male, 57 years old, right eye congestion and pain following injury, watering and reduced visual acuity for 20 days. Slit lamp examination shows irregular borders, infiltration and hypopyon. Fluorescent staining shows tear film accumulation.
 |
Click here to view |
Fig. 2: Case 2: Patient with chronic dacrocystitis and nasolacrimal duct obstruction, male, 65 years old, left eye congestion and throbbing pain following injury with vegetative matter. Matting of eyelashes, sticky discharge with corneal ulcer.
Total of 40 cases of fungal corneal ulcer were studied for a period of one year, out of which, 29(72.5%) cases were male and 11 (27.5%) cases were female. Patency of the lacrimal duct was determined by lacrimal sac syringing. Out of 40 cases of fungal corneal ulcer, 38 cases (95%) had patent nasolacrimal duct and only 2 cases (5.0%) had nasolacrimal duct obstruction. This finding is comparable to the study done by Li G et al where 3 cases of fungal corneal ulcer had concurrent nasolacrimal duct obstruction, out of which, two were female patients and one was male patient.[6]Association of fungal corneal ulcer with nasolacrimal duct obstruction was also noted in study done by Sun X et al.[10]
The two cases with fungal corneal ulcer in our study were male patients aged 57 years and 65 years respectively. This indicates higher incidence of nasolacrimal duct obstruction in older age group, similar to study done by Li G et al where the fungal corneal ulcer patients with concurrent nasolacrimal duct obstruction were 52 years, 67 years and 72 years old respectively. [6]
One male patient in our study had right eye involvement and the second male patient had left eye involvement. This is comparable to laterality displayed by fungal corneal ulcer patients of Li G et al study where left eye was involved in all the fungal corneal ulcer patients with concurrent nasolacrimal duct obstruction. [6]
In our study, both the patients were rural dwelling, similar to several studies done on fungal corneal ulcer demonstrating higher incidence of fungal corneal ulcers in rural dwelling population as they are predisposed to be exposed to dust contaminated with plant material.[11],[12],[13],[14]
All the 40 cases (100%) were KOH mount positive for fungal elements but only 9 cases (22.5%) were positive for fungal growth. Out of the 9 cases, 5(55.55%) displayed isolation of Fusarium species, 2(22.22%) showed Penicillium species, 1(11.11%) case showed Aspergillus and 1(11.11%) case showed growth of Curvularia which is a dematacious fungus. These findings are similar to study done by Jisha et al. [15]
Conclusion
Out of 40 cases of fungal corneal ulcer, 38 cases (95%) had patent nasolacrimal duct and only 2 cases (5.0%) had nasolacrimal duct obstruction. Though the incidence of fungal corneal ulcer with concurrent nasolacrimal duct obstruction is low, a thorough evaluation of lacrimal apparatus has to be performed and is essential in fungal corneal ulcer.
Conflict of Interest: None.
How to cite : Salagar K M, S.r Y, Concurrent lacrimal duct obstruction in patients with fungal corneal ulcer. IP Int J Ocul Oncol Oculoplasty 2019;5(1):12-14
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 2130
PDF Downloaded: 526