- Visibility 168 Views
- Downloads 24 Downloads
- DOI 10.18231/j.ijooo.2021.007
-
CrossMark
- Citation
Eye injuries in motor vehicle accidents: Epidemiology, spectrum of injury and analysis of risk factors
- Author Details:
-
Rajendra P Maurya *
-
Virendra Pratap Singh
-
C P Mishra
-
P Jain
-
Anil Kumar
-
Manish Kumar Prajapat
-
Sanjay Kumar Bosak
-
Eshwari Patel
-
Manisha
-
Shivani Verma
Introduction
Road traffic accidents (RTA) have been recognized as a major public health problem, causing high rates of mortality and morbidity. RTA is ranked eighth most common cause of death worldwide.[1] India accounts for almost 11% of the accident related deaths in the world.[2] In India number of RTA cases are increasing day by day due to the growing number of vehicles, new untrained drivers, congested and poor quality of roads and non-compliance to traffic rules. Road traffic accidents are responsible for a significant number of ocular injuries.[3] Though ocular injuries sustained in road traffic accidents are quite diverse, but are often associated with severe vision threatening complications. RTA related severe ocular trauma has significant impact on the individual, their family and society in terms of socioeconomic cost, morbidities, unnecessary toll on medical care, long term disability, loss of productivity, thereby affecting the quality of life. [3], [4] Permanent physical disfigurement and visual impairment can cause negative impact on physical as well as mental health of the victim. RTA is the most common cause of polytrauma and head, face and limbs are most frequently injured body parts. Orbit and maxilla are the most frequently fractured facial bones.[5], [6] The common vision threatening complications in RTA related ocular trauma is multiple complex orbital bone fractures, ruptured globe, intraocular haemorrhages, retinal detachment and optic nerve trauma, etc. Computed tomography scan (CT Scan) of face, orbit and skull with 3-dimensional reconstructed imaging is quite helpful in diagnosis and decision making.[7] It has been reported that about 90% of ocular trauma are preventable with the appropriate use of protective gear like safety glasses, helmet, seatbelt etc.[8] Lack of awareness of preventive measures and delay in immediate medical care, increases the chance of complications and subsequent visual disability and blindness.[9] Thus prevention should form the basis of management of ocular trauma. In order to formulate the preventive strategies, current clinico-epidemiological data related to ocular injuries caused by RTA is required. To date, no study has been reported from developing countries where the independent impact of characteristics of vehicle occupants and mode by accident on the RTA related eye injuries have been studied. Hence this hospital based study was conducted to evaluate the epidemiology, clinico-radiological pattern and visual outcome in patients having ocular injuries in road traffic accidents.
Materials and Methods
This was a prospective; hospital based, observational study conducted over a period of 5 years from March 2012 to February 2016 at SS hospital, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India. The study samples were collected from Trauma center, Ophthalmology and emergency outpatient department of the SS hospital after obtaining the ethics clearance from the research ethical committee of Institute of Medical Sciences, Banaras Hindu University. Patients of all age groups, both sexes having a road traffic accident related ocular trauma and giving consent were included in the study. Patients with ocular trauma >1 month, surgically treated elsewhere, having trauma other than RTA or those having co-existing vision threatening ocular diseases and those refused to participate were excluded from the study.
A prior informed consent was obtained from all the participants before enrollment. Meticulous history and thorough examination of all patients was done and the data were recorded in a predesigned, pretested proforma including demographic variables (age, sex, religion, residential area, marital status, occupation, per capita income, educational status of patients/parents), specific history of trauma (date, time, place and seasonal predilection of injury), type of road user(pedestrian or cyclist or two wheeler bike rider or car or bus occupant), type of road where accident occurred (pitch road or highway or mud road or brick road, etc.), number of vehicles involved, fate of the vehicle(overturned or skidded or run in a ditch or dashed against other objects like tree or wall or pole or other vehicles etc.), mode of injury (projectile object, fall, direct impact like frontal impact or sideways impact), the person’s cognitive state at the time of injury (drunken and sleepy) and information about the use of protective measures (seat belt/helmet etc.) at the time of injury were also noted. Patients were asked about initial complaints, present complaints, time elapsed between injury and treatment/consultation from outside and referral pattern. Patients were directly interviewed by the ophthalmologic team for specific ophthalmic treatment/surgery or admitted by other departmental staff and the ophthalmologic team was consulted. The patients were examined thoroughly to note the number of body parts involved, initial bed side visual acuity, severity of injury, extent of ocular injury (anterior segment/posterior segment involvement, type of globe injury & adnexal injury). Radiological investigations like USG B-scan & CT scan was done as per requirement. The patients were evaluated in deciding the treatment options and prognosis of globe injury was assessed by measuring ocular trauma score (OTS).
The collected data was entered into a spreadsheet and statistical analysis was performed using IBM SPSS (version 17.0 Chicago, USA: SPSS Inc). Categorical numerical variables were analyzed as frequency and percentage and chi-square test of significance was applied. P value <0.05 was considered as significant.
Results
Demographic profile and patient’s characteristics
Out of 402 ocular trauma cases during the study period, ninety-five patients (23.63%) injured due to RTA were included in the study. A total of 84(88.40%) patients were males and 11(11.60%) patients were females (p<0.01) which yielded a male to female ratio of 7.6:1, age ranged from 1 year to 67 years, with a mean and standard deviation of 30.53 ± 11.76 years. The most vulnerable age group was 21-30 years (25.30%) followed by 31-40 years (24.20%) and 11-20 years age group (21.10%)([Table 1]).
|
Characteristics |
Number of Victims |
Percentage (%) |
|
|
Total no of patients |
95 |
100.00 |
|
|
Sex |
Male |
84 |
88.40 |
|
|
female |
11 |
11.60 |
|
Age (in years) |
|
|
|
|
0-10 |
3 |
3.20 |
|
|
10-20 |
20 |
21.10 |
|
|
20-30 |
24 |
25.30 |
|
|
30-40 |
23 |
24.20 |
|
|
40-50 |
14 |
14.70 |
|
|
>50 |
11 |
11.60 |
|
|
Religion |
|
|
|
|
Hindu |
77 |
81.10 |
|
|
Muslim |
12 |
12.60 |
|
|
Others |
06 |
6.30 |
|
|
Marital status |
|
|
|
|
Married |
65 |
68.42 |
|
|
Single |
30 |
31.58 |
|
|
Educational status |
|
|
|
|
Illiterate |
32 |
33.68 |
|
|
Primary |
28 |
29.47 |
|
|
Middle |
15 |
15.79 |
|
|
Secondary |
10 |
10.53 |
|
|
Graduation & post-graduation |
10 |
10.53 |
|
|
Socioeconomic status |
|
|
|
|
Upper class |
10 |
10.53 |
|
|
Upper middle |
16 |
16.84 |
|
|
Middle class |
25 |
26.32 |
|
|
Lower middle class |
26 |
27.35 |
|
|
Lower class |
18 |
18.95 |
|
|
Habitat |
|
|
|
|
Rural |
40 |
42.10 |
|
|
Urban |
25 |
26.32 |
|
|
Semiurban |
30 |
31.58 |
|
|
Employment status |
|
|
|
|
Unemployed |
50 |
52.63 |
|
|
Employed |
22 |
23.16 |
|
|
Retired |
10 |
10.53 |
|
|
Unknown |
13 |
13.68 |
The majority of patients belonged to Hindu community (81.1%) and married (68.42%). Maximum number of victims belonged to rural background (42.10%) followed by semi urban (31.58%) and urban (26.32%) background. The majority of study subjects were either illiterate (33.68%) or having primary education (29.47%) only. Almost 52.63% victims were unemployed. Fifty one (53.68%) victims belonged to middle and lower middle socioeconomic status and 18.95% belonged to lower socioeconomic status ([Table 1]).
Injury profile
[Table 2] presents the information about circumstances of injury, conditions of roads, vehicles and victims during accidents. Most of the road accidents occurred in the summer (47.37%) season followed by winter (31.58%) and rainy (21.05%) seasons. The majority of the victims sustained injury in the afternoon period between 12.00 -17.59 hrs (29.47%) followed by in evening hours between 18.00-23.59 hrs (27.33%), in late night between 00:00 to 5:59 hours (22.11%) and in morning between 6:00 to 11:59 hours (21.05%). Commonest place of the accident was highway (43.16%) and pitch road (33.68%). However, in 12.63% cases accident occurred at poor quality mud/ kacchi roads in rural area. With regard to mode of travel during RTA is concerned, two wheeler riders (30.53%) are more prone for ocular injuries than those travelling in an auto-rikshaw (5.26%), four wheeler/car (21.05%) or pedestrians (13.68%). However, 29.47% of victims sustained ocular trauma while travelling through heavy vehicles like bus and truck. In the majority of cases (51.58%) vehicles dashed against other stationary objects like tree, mile post, pole, wall and another vehicle. Other fates of vehicle during RTA were swerved (15.79%), run in the ditch (13.68%) and skidded in 10.53% cases. The most common mode of oculofacial trauma was frontal impact (37.89%) followed by sideway impact (26.32%). In 6.32% victims, mode of ocular injury was projectile object while in 29.47% cases it was indeterminate. Alcohol influence was present in 42.11% of the vehicle drivers who sustained ocular injuries. The majority (57.89%) of victims were not using any protective device like helmet/seat belts at the time of injury. About 21.05% patients were sleepy during trauma.
|
Characteristics |
Number (N=95) |
Percentage (%) |
|
Time of injury |
|
|
|
06.00 -11.59 hrs |
20 |
21.05 |
|
12.00-17.59 hrs |
28 |
29.47 |
|
18.00 -23.59 hrs |
26 |
27.37 |
|
00:00-05.59 hrs |
21 |
22.11 |
|
Season of injury |
|
|
|
Summer |
45 |
47.37 |
|
Rainy |
20 |
21.05 |
|
Winter |
30 |
31.58 |
|
Type of road |
|
|
|
Mud (kacchi) road |
12 |
12.63 |
|
Pitch road |
32 |
33.68 |
|
Brick road |
10 |
10.53 |
|
Highway |
41 |
43.16 |
|
Mode of travel during accident |
|
|
|
Pedestrians |
13 |
13.68 |
|
2 wheeler and cyclist |
29 |
30.53 |
|
3 wheeler |
05 |
5.26 |
|
4 wheeler (car) |
20 |
21.09 |
|
4 wheeler (heavy vehicle) |
28 |
29.47 |
|
Fate of vehicle |
|
|
|
Overturned |
08 |
8.42 |
|
Swerved |
15 |
15.79 |
|
Skidded |
10 |
10.53 |
|
Run in ditch |
13 |
13.68 |
|
Dashed against other objects |
49 |
51.58 |
|
Mode of injury |
|
|
|
Projectile object |
06 |
6.32 |
|
Frontal impact |
36 |
37.89 |
|
Side way collision impact |
25 |
26.32 |
|
Indeterminate |
28 |
29.47 |
|
Alcohol influence among drivers |
|
|
|
Present |
40 |
42.11 |
|
Absent |
37 |
38.94 |
|
Indeterminant |
18 |
18.94 |
|
Use of protective devices during RTA |
|
|
|
Yes |
40 |
42.11 |
|
No |
55 |
57.89 |
|
Sleepy/drowsiness of driver |
|
|
|
Yes |
20 |
21.05 |
|
No |
60 |
63.16 |
|
Unknown |
15 |
15.79 |
Clinical profile
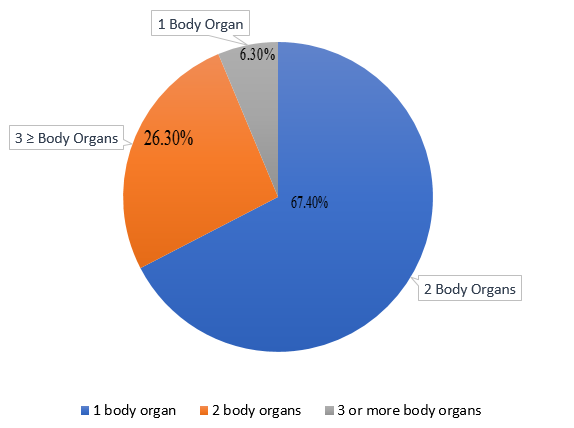
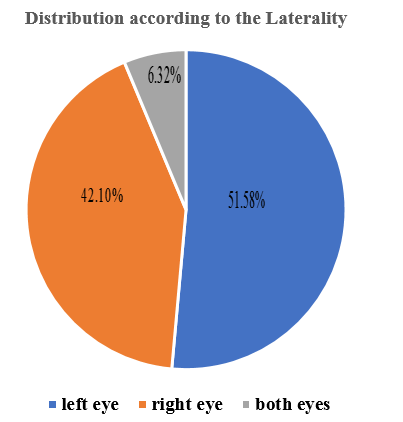
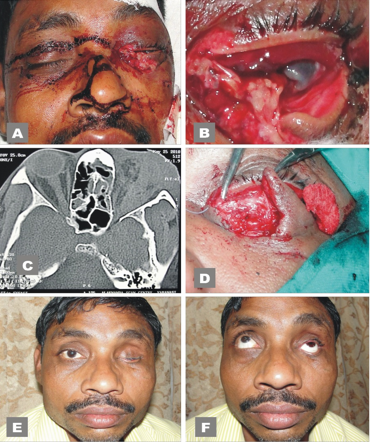
[Figure 1] shows only 6.30% injury victims had isolated ocular trauma and rest (93.70%) had polytrauma. Among them majority (67.40%) had two body organ involvement and 26.30% had ≥ 3 body organ involvement. Common multiple organ involvement were maxillofacial and eye injury (49.50%), head and eye injury (18.81%). Out of 95 RTA patients 89(93.68%) had unilateral involvement and rest 6(6.32%) had bilateral eye injuries. There was a predominance of left eye (51.58%) involvement ([Figure 2]).
In the present study 101 eyes of 95 patients had RTA related ocular injury. Among them, most common ocular part involved was eyelid/periocular skin (85.15% eyes) followed by conjunctiva (82.18% eyes), eye ball in 68(71.58% eyes) and orbit in 51.49% eyes ([Table 3]).
|
Ocular involvement |
Number of eyes |
Percentage |
|
Orbital |
52 |
51.49 |
|
Eyelids/periocular |
86 |
85.15 |
|
Conjunctiva |
83 |
82.18 |
|
Cornea |
39 |
38.61 |
|
Sclera |
36 |
35.64 |
|
Anterior chamber |
28 |
27.72 |
|
Pupil |
31 |
30.69 |
|
Lens |
20 |
19.80 |
|
Vitreous |
19 |
18.81 |
|
Retina |
23 |
22.77 |
|
Optic nerve |
11 |
10.89 |
[Table 4] presents type of eyeball injury. Out of total 101 injured eyes, 36 (35.64%) eyes had an open globe injury and 32(31.68%) eyes had closed globe injury. The most common type of open globe injury were ruptured globe (21.78% eyes) and majority of open globe injury belonged to zone II (14.84% eyes) and zone III (10.89% eyes) injury. Among the closed globe injury maximum eyes belonged to zone I (9.90%) and zone II (15.84%) injury).
|
Types of globe injury |
Number of eyes |
Percentage |
|
Open globe injury |
36 |
35.64 |
|
Zone I |
10 |
9.90 |
|
Zone II |
15 |
14.85 |
|
Zone III |
11 |
10.89 |
|
Closed globe injury |
32 |
31.68 |
|
Zone I |
06 |
5.94 |
|
Zone II |
16 |
15.84 |
|
Zone III |
10 |
9.90 |
Type of ocular injuries in study subjects is given in [Table 5]. Commonest type of ocular injury was ecchymosis (77.23% eyes) followed by eyelid & periocular laceration (67.33% eyes), globe injury (67.33% eyes), sub-conjunctival haemorrhage (59.41% eyes), orbital fracture (51.49 % eyes), hyphema (41.58% eyes) and lens injury (31.68% eyes) ([Figure 3]). Commonest posterior segment injury was vitreous haemorrhage (24.70% eyes) followed by retinal detachment (15,84% eyes) and traumatic optic neuropathy (5.94% eyes).
|
Types of ocular trauma |
Number of eyes (n=101) |
Percentage |
|
Ecchymosis |
78 |
77.23 |
|
Eyelid & periocular laceration |
68 |
67.33 |
|
Orbital fracture |
52 |
51.49 |
|
Subconjunctival haemorrhage |
60 |
59.41 |
|
Penetrating injury |
14 |
13.86 |
|
Rupture globe |
22 |
21.78 |
|
Hyphema |
42 |
41.58 |
|
Iridodialysis |
22 |
21.78 |
|
Lens dislocation/subluxation |
16 |
15.84 |
|
Traumatic cataract |
16 |
15.84 |
|
Vitreous haemorrhage |
25 |
24.75 |
|
Retinal detachment |
16 |
15.84 |
|
Choroidal tear |
04 |
3.96 |
|
Traumatic optic neuropathy |
06 |
5.94 |

[Table 6] depicts the distribution of study subjects according to type of orbital fracture. Out of 52(51.49%) eyes having orbital fracture, 42.31% was associated with maxillofacial fracture, 19.23% had acranio-orbital fracture and 25.00% eyes were having cranio-orbitofacial trauma. However 13.40% eyes had isolated orbital wall fracture.5.26% victims had bilateral orbital fracture. Most of the injured eyes had three orbital wall fracture (38.46%) and two orbital wall fracture (28.85%) while 19.23% eyes had a single orbital wall fracture and 13.46% had pan-orbital wall fracture ([Figure 4]). Most common orbital wall fracture was floor fracture (34.61% eyes) followed by fracture medial wall (30.77% eyes) and fracture roof of orbit (23.08%). However, fracture lateral orbital wall was only seen in 11.84% eyes.
|
Types of orbital trauma |
Number of eyes |
Percentage |
|
Isolated orbital trauma |
07 |
13.46 |
|
Maxillofacial-orbital trauma |
22 |
42.31 |
|
Cranio-orbital trauma |
10 |
19.23 |
|
Cranio-orbitofacial trauma |
13 |
25.00 |
|
Number of orbital wall fracture |
|
|
|
One wall |
10 |
19.23 |
|
Two wall |
15 |
28.85 |
|
Three wall |
20 |
38.46 |
|
Pan-orbital fracture |
07 |
13.46 |
|
Location of fracture |
|
|
|
Inferior wall(floor) |
18 |
34.61 |
|
Medial wall |
16 |
30.77 |
|
Superior wall |
12 |
23.08 |
|
Lateral wall |
06 |
11.54 |
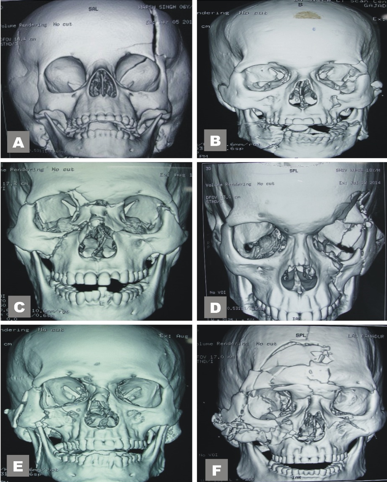
The majority of patients (83.16%) required multidisciplinary treatment, however 16.84% patients treated by only ophthalmic surgeon. 8.4% patients underwent multiple ocular surgeries ([Figure 5], [Figure 6]).
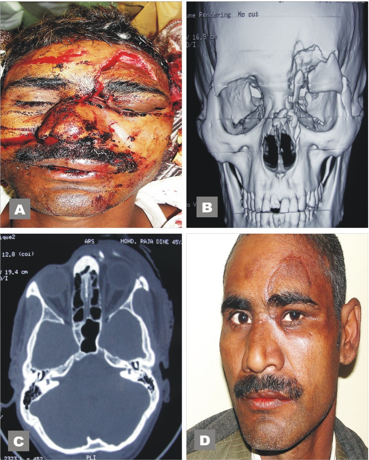
Upon initial presentation 40 eyes (39.60%) had visual impairment (VA<6/18-6/60) and 22 eyes (21.78%) had blindness (VA<6/60-NO PL) while the visual acuity could not be assessed in 12(11.88%) eyes. On final follow up, the number of visually impaired eyes fell down to 31(30.69%) and blinding outcome was found in 26(25.74%) eyes [[Table 7]]. Visual outcome was directly proportional to the number of orbital wall fracture. Severe visual loss was observed in eyes having ≥2 orbital wall fracture [[Table 8]].
|
Visual Acuity |
Initial |
Final |
||
|
|
No |
Percentage |
No |
Percentage |
|
6/6 -6/18 |
27 |
26.73 |
30 |
29.70 |
|
<6/18-6/60 |
40 |
39.60 |
31 |
30.69 |
|
< 6/60-NPL |
22 |
21.78 |
26 |
25.74 |
|
Unknown |
12 |
11.88 |
14 |
13.86 |
|
Visual acuity |
Single wall fracture |
Two wall fracture |
Three wall fracture |
Pan-orbital wall fracture |
||||
|
|
No |
% |
No |
% |
No |
% |
No |
% |
|
6/60-6/18 |
4 |
7.69 |
2 |
3.85 |
2 |
3.85 |
• |
- |
|
<6/18-6/60 |
3 |
5.77 |
8 |
15.38 |
14 |
26.92 |
5 |
9.61 |
|
<6/60-NOPL |
3 |
5.77 |
1 |
1.92 |
2 |
3.85 |
1 |
1.92 |
|
Unknown |
- |
- |
|
|
|
|
• |
|
|
Total |
10 |
19.23 |
15 |
28.85 |
20 |
38.46 |
7 |
13.46 |
Discussion
Road Traffic Accidents (RTA) a major cause of vision loss in young adult population. Ocular trauma due to RTA is common in both developed and developing countries with different risk factors. Factors responsible for RTA related ocular injuries include human factors (like age, sex, physical impairment, alcohol or any drug intoxication while driving, etc), environmental factors (like season and weather conditions), time of injury (night driving), condition of the road, vehicle factors (like the type of vehicle, speed of vehicle, safety design of the vehicle) and mode by accident etc.
In this Hospital based observation study, Out of 402 ocular trauma patients, 95 patients (23.63%) were injured due to RTA. The variable incidence of RTA related ocular injuries have been reported in previous studies, like Canavam et al[10] (32.5%), Georgouli et al[11] (56%), Mackay et al[12] (70%), Laila et al[13] (60.7%) and El Shtewi M, et al[14] (12.5%). It has been reported that young adult males have a high risk of ocular injury in an RTA.
In this study, male patients (88.40%) had more ocular injuries as compared to females (11.6%) with M:F ratio being 7.6:1. Other researchers also reported a male predominance like El Shtewi M, et al[14] from Libya reported 75% male and 25% female injury victims, Jonston et al[15] from Northern Ireland reported RTA related ocular injuries in 72.20% of his male patients and 27.20% of his female patients, and Kumar J, et al[16] from India reported incidence as 77.6%in males and 22.4% in females, Arora et al[17] from India also reported M: F ratio to be 2.5:1. This higher incidence of ocular trauma in an RTA in men can be explained by their more outdoor activities with increased travelling and rash driving.
In our study, the most vulnerable age group was between 21-30 years (25.3%) followed by 31-40 years age group (24.2%) and 11-20 years (21.1%). Similar peak age of 21-30 years were also reported by Alam J, et al[18] from India. Ezegwvi et al[19] and Arora et al have also reported similar peak age (16-30years) in their study. However Muralidhar et al[20] reported higher peak age (41-50 years) than that reported in most of literature and they gave an explanation saying that in South India even elderly persons are also bread winners of the family. This is obvious from the present study that vulnerability in ocular trauma is more common in young adults and productive age group and this decreased in extreme, dependent age group.
In this study, we observed that the incidence of RTA related ocular trauma was higher in summer season (47.37%) than in the winter season (31.58%) and rainy season (21.05%) showing seasonal trends in the occurrence of RTA. In India summer season is a season of marriage and school holidays and more people travelling on the road. In winter, season, cold and foggy climate limits the close visibility and may cause vehicular collision. In such climate, vehicles with fog lamp and slow speed can minimize the accident. Maximum RTA occurred on a week-ends and during afternoon (29.47%) and in the night time. The afternoon is the time for outdoor activity and productive hours of every individual and during the night most of the drivers facing difficulties in driving due to glare caused by headlights, and also complain fatigue and sleepiness.
In this study, it is observed that two-wheeler riders (30.53%) were more prone to ocular injuries than three-wheeler riders (5.26%), car-occupants (21.05%) and pedestrian (13.68%). However Madhuramuthu et al[21] from India reported that 87.33% and Kumar J et al[16] reported that 73.6% of ocular injuries occurred in two-wheeler riders. The majority of accidents occurred either on the highways or on the pitch road. In most of the accident cases, a vehicle crashed against other stationary objects like a tree, pole or another vehicle. The commonest mode of injury was a frontal collision (37.89%) followed by sideways impact (26.32%). In car occupants, driver and who rode on the left front seat sustained severe ocular injuries than those who rode with a middle seat.
In this study, it is also seen that 53.89% of two-wheeler riders were not wearing helmet and none of the car occupants were wearing seatbelt while riding. It has been reported that after compulsory seatbelt wearing legislation was introduced in car driving, a 60-75% reduction in RTA related ocular injuries was observed.[22] Thus travelling without wearing protective gears (helmet and seat-belts) is one of the major modifiable risk factors for RTA related ocular injuries.
In our study, driving under the influence of alcohol was noticed in 42.10 % of drivers. Similar observations were also reported by Alam J, et al.[18] However, Kumar J et al[16] reported that 71.2% of drivers who sustained ocular injuries were under the influence of alcohol while driving. Thus driving under the influence of alcohol is another risk factor for RTA related ocular injuries.
RTA related eye injuries are frequently associated with polytrauma. In this study only 6.30% injury victims had isolated ocular trauma rest had multiple organ involvement. Commonest involved organs were face and skull. Majority (93.68%) of the victims had unilateral ocular involvement. The reported incidence of bilateral ocular involvement among RTA related ocular injuries varies from 4% to 50%; Briner et al[23] (4%), Kriedl et al[24] (4.9%), Kumarasamy et al[25] (9.7%), Taylor et al[26] (50%). In this study there was a slight predominance of left eye (51.58%) involved. However, previous studies reported higher proportion of right eye injury.[14], [17], [20], [25], [27] The important prognostic factors of an eye injury are ocular tissue involvement. The posterior segment injury has a worse prognosis than trauma confined to the anterior segment. Out of 101 eyes, orbital injury was seen in 51.49% eyes. Eyelids were involved in 85.15% eyes, conjunctiva in 82.18% eyes and globe injury in 67.33% eyes. The posterior segment injury was noticed in 52.48% eyes. Similar finding was reported by Kumarsamy et al.[25] In our study, commonest ocular injury was ecchymoses (77.23% eyes) followed by eyelid laceration (67.33%), subconjunctival haemorrhage (51.41% eyes) and globe injury (67.33%). KumarJ et al[16] reported periorbital oedema with ecchymoses (82.2%) followed by eyelid laceration (68.8%) as a commonest type of injury. Similar findings were also reported by Alam J et al[18] and Kumarsamy et al.[25] The commonest ocular injury reported by Muralidhar et al [20] was subconjunctival haemorrhage followed by ecchymoses. Orbit and periocular structures are the first structures to take impact of the injury in accident.
Open globe injury specially rupture globe is one of the major risk factors for poor visual outcome because it always requires surgeries which may be difficult and may lead to long term visual impairment.[28], [29] In our study open globe injury (35.64%) was more common than closed globe injury (3168%). While other studies reported high incidence of closed globe injury in RTA; Mishra A et al[30] (86.4%), Marudhamuthu et al[21] (95.34%), Smith et al[31] (68.58%) and Kumarsamy et al[25] (95.13%). In this study, the commonest type of open globe injury was a rupture globe in 21.78% eyes and rest 13.86% eyes had penetrating injury leading to corneoscleral laceration. Majority of open globe injury fell in zone II (11.18% eyes) and zone III (19.8% eyes) injuries. Various studies have demonstrated that zone II and zone III injuries are risk factors likely to predict poor visual prognosis.[32], [33], [34]
In our study 52 eyes of 48 (50.53%) patients had orbital fractures. Cruz et al [35] reported RTA related orbital fractures in 54% of patients and Kumarsamy et al [25] found orbital fractures in 22.22% of study subjects. While in study of Shtewi et al [14] only 1.1% of victims presented with orbital fracture. The isolated orbital fracture was seen in 13.46% cases only and rest of the patients had associated fractures of facial and cranial bones. Most of the injured eyes had three orbital wall (38.46%) and two orbital wall fractures (28.85%) while 13.46% eyes had pan orbital wall fractures. In our study, inferior wall (34.61% eyes) and medial wall (30.77%) fractures were more common. Least commonly fractured orbital wall was lateral wall (6/52, 11.54% eyes) because the lateral wall is strongest orbital wall. However, in study of Marudhamuthu et al,[21] the lateral wall fracture was common (8 out of 14 orbital fracture cases). His explanation being the major force coming from the sideways impact in an RTA. In this study, about 50% of patients having rupture globe had associated multiple orbital wall fractures. In the study done by Chen X et al,[36] out of 197 eyes of a rupture globe, 32 eyes got injured due to RTA. Among them 15 eyes had rupture globe with orbital fracture. In the present study 4.22% of patients with rupture globe required enucleation. While previous studies showed that 5-23% of open globe injury patients required excision of globe.[5], [15], [37] In road traffic accident case, orbital fracture may lead to severe loss of vision.[38]
In our study, 29.70% eyes had good visual outcome and 30.69% eyes had visual impairment. However, blinding outcome was found in 25.74% eyes. Visual outcome was directly proportional to the number of orbital walls fractured. We noticed that blinding outcome was maximum in eyes having more than 2 orbital wall fracture. Above findings suggested that orbital fracture could be an independent risk factor for poor prognosis in RTA related eye injuries. Above findings also explained that ruptured globe with orbital fractures is a severe type of eye injury that may carry a worse prognosis.
Few limitations of our study should be acknowledged and discussed. First, as it is a hospital based study, therefore trends cannot be stipulated directly to the community and a nationwide eye injury surveillance system should be established. Second being relatively small size for internal subgroup comparison. Another limitation of this study is being whether delayed presentation is related to visual outcome or not was not assessed. However, these limitations do not significantly affect the major findings of this study.
Conclusion
In conclusion, RTA can cause severe ocular trauma. Victims are usually adult males of the productive age group. Two wheeler riders, frontal impact, alcohol consumption, non use of safety measures and not following traffic rules are major risk factors. We found several other prognostic factors for poor visual outcome; ruptured globe with zone II or III injury, multiple orbital fractures, intraocular haemorrhage and posterior segment trauma, poor initial visual acuity. Public health education regarding use of helmet & seat belt, early reporting and appropriate intervention may reduce the vision threatening complications & blindness in RTA related ocular trauma.
Ethical Clearance
The study received ethical clearance from the Institute of medical Sciences, Banaras Hindu University.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- . Road traffic injuries-World Health Organisation. . [Google Scholar]
- . Road accidents in India-2019./Ministry of Road Transport & Highways. . . [Google Scholar]
- R P Maurya, T Srivastav, VP Singh, CP Mishra, A Al-Mujaini. The epidemiology of ocular trauma in Northern India: A teaching hospital study. Oman J Ophthalmol 2019. [Google Scholar] [Crossref]
- A.-D. Négrel, B. Thylefors. The global impact of eye injuries. Ophthalmic Epidemiol 1998. [Google Scholar] [Crossref]
- D FHuelke, J OʼDAY, WH Barhydt. Ocular Injuries in Automobile Crashes. J Trauma 1982. [Google Scholar] [Crossref]
- D F Huelke, W C Grabb, R O Dingman. Facial injuries in automobile accidents. In Proceedings, American association for automotive medicine, Louisville. 1964. [Google Scholar]
- R P Maurya, V P Singh, M K Singh, Shrinkhal, P R Sen, A Verma. Diagnostic value of three-dimensional reconstruction in various orbital disorders. IP Int J Ocul Oncol Oculoplast 2016. [Google Scholar]
- LD Pizzarello. Ocular trauma: time for action. Ophthalmic Epidemiol 1998. [Google Scholar] [Crossref]
- C G Thompson. The aetiology of perforating ocular injuries in children. Br J Ophthalmol 2002. [Google Scholar] [Crossref]
- Y. M. Canavan, M. J. O'Flaherty, D. B. Archer, J. H. Elwood. A 10-year survey of eye injuries in Northern Ireland, 1967-76.. Br J Ophthalmol 1980. [Google Scholar] [Crossref]
- T. Georgouli, I. Pountos, B. Y. P. Chang, P. V. Giannoudis. Prevalence of ocular and orbital injuries in polytrauma patients. Eur J Trauma Emerg Surg 2011. [Google Scholar] [Crossref]
- G M Mackay. Incident of trauma to the eyes of car occupants. Trans Ophthalmol soc UK 1975. [Google Scholar]
- LT Ababneh, H Mohidat, H Abdelnabi, M F Kana’an, N A Tashtush, O S El-Mulki. Hospital-Based Ocular Trauma: Factors, Treatment, And Impact Outcome. Clin Ophthalmol 2019. [Google Scholar] [Crossref]
- M El Shtewi, M N Shishko, G K Purohit. Road traffic accidents and ocular trauma: experience at Tripoli Eye Hospital, Libya. Community Eye Health 1992. [Google Scholar]
- P. B. Johnston, M. F. Armstrong. Eye injuries in Northern Ireland two years after seat belt legislation.. Br J Ophthalmol 1986. [Google Scholar] [Crossref]
- J Kumar, V P Singh, P Chaubey, V Kumar. Ocular injuries in road traffic accidents (RTA). J Dent Med Sci 2017. [Google Scholar]
- A S Arora, Gajesh Bhargava, Aravind Chauhan. Ocular trauma in road traffic accidents: Experience at Mathra Das Hospital. Rajasthan J Ophthalmol 2011. [Google Scholar]
- J Alam, H Bhattacharjya, A Roy, M Das. Epidemiology and outcome of ocular trauma among the road traffic accident cases attending a tertiary care hospital in Tripura. Int J Med Sci Public Health 2014. [Google Scholar] [Crossref]
- I R Ezegwui. Eye injuries during road traffic accidents at Abakaliki, Nigeria. Int J Ophthalmol 2004. [Google Scholar]
- P Muralidhar, N L Chowdary. Ocular manifestations in road traffic accidents: A study done at a medical college hospital in South India. Int J Contemp Med Reas 2016. [Google Scholar]
- E Marudhamuthu, N Sivakumar, T Kumaravel. Study of ocular injuries in road traffic accident patients. J Evol Med Dent Sci 2017. [Google Scholar] [Crossref]
- W Schrader, E Gramer, F Goldmann, U Marcus. Penetrating and perforating eye injuries in 343 patients due to auto accidents before and after compulsory seat belt legislation resulting in fines. Klin Monatsbl Augenheilkd 1966. [Google Scholar]
- A M Briner. Penetrating eye injuries associated with motor vehicle accidents. Med J Aust 1976. [Google Scholar]
- KO Kreidl, DY Kim, SE Mansour. Prevalence of significant intraocular sequelae in blunt orbital trauma. Am J Emerg Med 2003. [Google Scholar] [Crossref]
- R Kumarasamy, U Velpandian, H Anandan. Visual outcome in ocular injuries in road traffic accident. Int J Sci Study 2016. [Google Scholar]
- WOA Taylor. Car seat belts and the eye. Plast Reconstr Surg 1975. [Google Scholar] [Crossref]
- R Koval, J Teller, M Belkm, M Romem, L Yanko, H Savir. The Israeli ocular injury study. A nationwide collaborative study. Arch Ophthalmol 1988. [Google Scholar] [Crossref]
- C H Lee, W Y Su, L Lee, M L Yang. Pediatric Ocular trauma in Taiwan. Chang Gung Med J 2008. [Google Scholar]
- Cao He, L Li, M Zhang, H Li. Epidemiology of pediatric ocular trauma in the Chaoshan Region. Plos one 2001. [Google Scholar]
- A Mishra, J Parihar, AK Verma, S Aggarwal, VK Baranwal, N Bhargava. The pattern and visual outcomes of ocular trauma in a large zonal hospital in a non-operational role: A 36 months retrospective analysis. JClin Ophthalmol Res 2014. [Google Scholar] [Crossref]
- ARE Smith, SB O'Hagan, GA Gole. Epidemiology of open- and closed-globe trauma presenting to Cairns Base Hospital, Queensland. Clin Exp Ophthalmol 2006. [Google Scholar] [Crossref]
- B Knyazer. Open globe eye injury characteristics and prognostic factors in Southern Israel: A retrospective epidemiologic review of 10 years experience. Israel Med Associ J 2013. [Google Scholar]
- Y Meng, H Yan. Prognostic Factors for Open Globe Injuries and Correlation of Ocular Trauma Score in Tianjin, China. J Ophthalmol 2015. [Google Scholar] [Crossref]
- R Agrawal, HS Wei, S Teoh. Prognostic factors for open globe injuries and correlation of Ocular Trauma Score at a tertiary referral eye care centre in Singapore. Indian J Ophthalmol 2013. [Google Scholar] [Crossref]
- A A V Cruz, GCD Eichenberger. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol 2004. [Google Scholar] [Crossref]
- X Chn, Y Yao, F Wang, T Liu, X Xiao. A retrospective study of eyeball rupture in patients with or without orbital fracture. Medicin 2017. [Google Scholar]
- K G Soni. Eye injuries in road traffic accidents. Injury 1973. [Google Scholar]
- R P Maurya, P Jain, V P Singh, M K Singh, C P Mishra, A Verma. Etiology and pattern of orbital fractures in a teaching hospital. IP Int J Ocul Oncol Oculoplast 2017. [Google Scholar]
How to Cite This Article
Vancouver
Maurya RP, Singh VP, Mishra CP, Jain P, Kumar A, Prajapat MK, Bosak SK, Patel E, Manisha , Verma S. Eye injuries in motor vehicle accidents: Epidemiology, spectrum of injury and analysis of risk factors [Internet]. IP Int J Ocul Oncol Oculoplasty. 2025 [cited 2025 Sep 05];7(1):30-39. Available from: https://doi.org/10.18231/j.ijooo.2021.007
APA
Maurya, R. P., Singh, V. P., Mishra, C. P., Jain, P., Kumar, A., Prajapat, M. K., Bosak, S. K., Patel, E., Manisha, , Verma, S. (2025). Eye injuries in motor vehicle accidents: Epidemiology, spectrum of injury and analysis of risk factors. IP Int J Ocul Oncol Oculoplasty, 7(1), 30-39. https://doi.org/10.18231/j.ijooo.2021.007
MLA
Maurya, Rajendra P, Singh, Virendra Pratap, Mishra, C P, Jain, P, Kumar, Anil, Prajapat, Manish Kumar, Bosak, Sanjay Kumar, Patel, Eshwari, Manisha, , Verma, Shivani. "Eye injuries in motor vehicle accidents: Epidemiology, spectrum of injury and analysis of risk factors." IP Int J Ocul Oncol Oculoplasty, vol. 7, no. 1, 2025, pp. 30-39. https://doi.org/10.18231/j.ijooo.2021.007
Chicago
Maurya, R. P., Singh, V. P., Mishra, C. P., Jain, P., Kumar, A., Prajapat, M. K., Bosak, S. K., Patel, E., Manisha, , Verma, S.. "Eye injuries in motor vehicle accidents: Epidemiology, spectrum of injury and analysis of risk factors." IP Int J Ocul Oncol Oculoplasty 7, no. 1 (2025): 30-39. https://doi.org/10.18231/j.ijooo.2021.007
